Questions:
1. Where is the horizontal gaze center located?
2. What is the location of the burst neurons responsible for horizontal saccades?
3. What are the findings of a lesion of the 6th nerve nucleus?
4. What are the findings of a lesion of the PPRF?
5. What are 4 findings of a unilateral internuclear ophthalmoplegia?
6. Where is the lesion located that produces a unilateral internuclear ophthalmoplegia?
7. What are the findings of a bilateral internuclear ophthalmoplegia?
8. What are the findings of a walleyed bilateral internuclear ophthalmoplegia (WEBINO)?
9. Where is the lesion located that produces a wall-eyed bilateral internuclear ophthalmoplegia (WEBINO)?
10. What are the findings of the One-and-a-Half Syndrome?
11. Where is the lesion located that produces the One-and-a-Half Syndrome?
12. What are 2 common causes of isolated internuclear ophthalmoplegia?
13. What conditions may mimic an isolated internuclear ophthalmoplegia?
14. What conditions may mimic the one-and-a-half syndrome?
Archives for 2018
Neuro-ophthalmology questions of the week: NOI13 Diplopia 9.1 – Internuclear & Supranuclear Lesions
Clinical Reasoning: A 64-year-old man with painful, unilateral external ophthalmoplegia
Clinical Reasoning: A 64-year-old man with painful, unilateral external ophthalmoplegia
M. Tariq Bhatti. Neurology. 2010; 75 (8)
RESIDENT AND FELLOW SECTION
SECTION 1
A 64-year-old man was referred for evaluation of double vision in March 2009. Four months prior, he experienced daily pain in the region of the right forehead and right eye. Two months later, he noticed constant binocular, vertical double vision. Evaluation by an outside ophthalmologist resulted in the diagnosis of a right 4th cranial nerve (CN) palsy, a normal cranial and orbital MRI study with contrast, and an unremarkable laboratory evaluation. One month later, his right eye began “turning in,” and within a few days he was unable to abduct the eye. Several weeks later, the right eyelid began to droop and progressively worsened over the next several days to complete closure of the eye.
His past medical history was notable for arterial hypertension, depression, rheumatoid arthritis, gastroesophageal reflux disease, nephrolithiasis, squamous cell carcinoma of the forehead, and a precancerous melanoma of the left ear.
When he was seen in the neuro-ophthalmology clinic, visual acuity was 20/20 in each eye. Color vision was intact in each eye. The right pupil was 2 mm larger than the left and was nonreactive to light or near effort. There was no relative afferent pupillary defect (RAPD). Dilated fundus examination was normal in each eye. Eye movements of the right eye were limited in all directions and there was complete right upper eyelid ptosis (figure 1). Corneal sensation of the right eye was absent and there was numbness over the right forehead. The remainder of the cranial nerve examination was normal.
Figure 1 Nine cardinal positions of eye movements
There is limited movement of the right eye in all directions of gaze. There was no intorsion of the right eye on attempted downgaze. The right eyelid is manually elevated because of the complete right eyelid ptosis (center, middle panel). Permission obtained from patient.
Questions for consideration:
1. What is the clinical presentation?
2. Where does the lesion localize?
Neuro-ophthalmology Question of the week: NOI13 Diplopia 8 Multiple Cranial Nerve Involvement
Questions:
1. What associated signs with lesions causing unilateral or bilateral ophthalmoplegia may help localize the lesion
2. What are the findings of the orbital apex syndrome?
3. What are the findings of the cavernous sinus syndrome?
4. Do brainstem lesions commonly produce multiple cranial nerve palsies?
5. What are 7 systemic disorders that affect the cranial nerves?
6. What condition should be considered in patients with unilateral or bilateral ophthalmoplegia and normal pupils presumed to result from multiple cranial neuropathies?
7.What should be presumed to be the cause of a painful orbital apex syndrome in a diabetic patient?
8. Do normal orbital imaging studies rule out an orbital apex lesion?
9. Does the orbital apex syndrome involve V2?
10. Which cranial nerves are enclosed in the lateral wall of the cavernous sinus?
11. Why do cavernous carotid artery aneurysms often present with an isolated sixth nerve palsy?
12. What diagnoses should be considered in all cases of new onset constant or transient ptosis and/or diplopia
13. What syndromes have ataxia, areflexia and ophthalmoplegia?
14. What is the Guillain-Barré syndrome?
15. What is the Miller Fisher syndrome?
16. What is the difference between the Miller Fisher and the Guillain-Barré syndromes?
17. When should the Wernicke encephalopathy be considered and what are its symptoms?
18. What is the cause and treatment of Wernicke encephalopathy?
19. What does botulism do to the pupils and what are its other symptoms?
20. What is the infectious agent of botulism?
21. What is the mechanism of the botulism toxin?
22. What is the treatment for botulism?
Teaching NeuroImages: Herpes zoster ophthalmicus–related oculomotor palsy accompanied by Hutchinson sign
Teaching NeuroImages: Herpes zoster ophthalmicus–related oculomotor palsy accompanied by Hutchinson sign
Gayatri S. Reilly and Robert K. Shin
Neurology. April 13, 2010; 74 (15) RESIDENT AND FELLOW SECTION
ARTICLE
A 51-year-old woman presented with acute diplopia. Findings include right ptosis, a dilated, unreactive pupil, and impaired adduction and vertical ductions (figure 1). A skin lesion was noted on the right tip of the nose, residual from a vesicular rash over the right forehead 3 weeks earlier (figure 1). MRI demonstrated enhancement of the cisternal third nerve, obviating the need for angiography (figure 2). The oculomotor palsy resolved within 3 months.

Figure 1 Partial ptosis, mydriasis, and exotropia consistent with a right oculomotor palsy
The skin lesion on the tip of the nose (Hutchinson sign) signifies involvement of the nasociliary branch of V1, which also innervates ocular structures.
Neuro-ophthalmology Questions of the week: NOI13 Diplopia 7 – 3rd Nerve Palsy
Questions:
1. How are 3rd nerve dysfunctions classified?
2. What is the definition of a partial 3rd nerve palsy?
3. What are the two categories of complete 3rd nerve palsies?
4. What is meant by “a pupil-sparing 3rd nerve palsy”?
5. What tests should be done when a patient over age 50 presents with an isolated incomplete 3rd nerve palsy and the pupil is involved?
6. What should be done when a patient over age 50 presents with an isolated complete 3rd nerve palsy and the pupil is NOT involved?
7. What should be done when a patient over age 50 presents with an isolated complete 3rd nerve palsy, the pupil is NOT involved, and has normal lab (Blood glucose, CBC, platelets, ESR, CRP) is followed daily and develops pupillary involvement?
8. What is the most common cause of an isolated “pupil-sparing 3rd nerve palsy”?
9. Are microvascular 3rd nerve palsies painful?
10. What should be ruled-out when making the diagnosis of a microvascular complete 3rd nerve palsy with pupil-sparing in a patient over 50?
11. What in addition to cranial arteritis should be considered when making the diagnosis of a microvascular pupil complete 3rd nerve palsy with pupil-sparing?
12. How long does it usually take for a microvascular 3rd nerve palsy to resolve?
13. If a complete 3rd nerve palsy with pupil-sparing thought to be of microvascular origin does not clear in 4 months what should be done?
14. What test should be done in a patient under age 50 who presents with an isolated 3rd nerve palsy with or without pupillary involvement?
15. Should the pupils of a patient with an acute 3rd nerve palsy with “pupil sparing” be dilated to complete the eye exam?
16. What should be ruled-out in a patient without a history of trauma has signs of aberrant regeneration of the 3rd nerve?
17. What are the symptoms of pituitary apoplexy?
18. What are the findings when there is a unilateral lesion of the entire 3rd nerve nucleus?
19. Why does a complete unilateral nuclear 3rd nerve palsy have bilateral ptosis?
20. Why does a complete unilateral nuclear 3rd nerve palsy have bilateral elevation deficits?
21. What are the findings of a unilateral lesion of the 3rd nerve fascicle?
Teaching NeuroImages: Upright-supine test to evaluate vertical diplopia
Teaching NeuroImages: Upright-supine test to evaluate vertical diplopia
Nailyn Rasool and Sashank Prasad
Neurology May 12, 2015; 84 (19)
RESIDENT AND FELLOW SECTION
Article:
A 36-year-old woman presented with vertical diplopia, nausea, and disequilibrium. Maddox rod testing was performed in the upright and supine positions (figures 1 and 2).
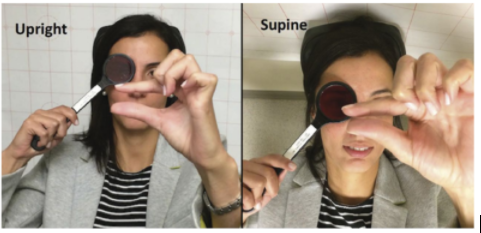
Figure 1 Upright-supine test
During Maddox rod testing, the patient used her fingers to demonstrate the separation of images.
The vertical deviation decreased substantially (over 50%) when supine compared to upright.
Questions of the Week: NOI13 Diplopia 6 – 4th Nerve Palsy
NOI13 Diplopia 6 – 4th Nerve Palsy
Questions:
63. What are 6 characteristics of a 4th nerve palsy?
64. When a patient has a 3rd nerve palsy and the eye cannot adduct, how can the function of the ipsilateral 4th nerve shown to be present?
65. What other conditions should be considered when the patient has the findings of a 4th nerve palsy?
66. A patient has a 4th nerve lesion associated with a contralateral Horner syndrome, where does this localize the lesion?
67. A microvascular 4th nerve palsy is suspected because a 60-year-old patient has diabetes, hypertension and hyperlipidemia what should be ordered?
68. A presumed microvascular 4th nerve palsy in a 60-year-old patient with diabetes, hypertension and hyperlipidemia has not resolved within 3-6 months, what test should be ordered?
69. A 60 year-old patient presents with intermittent vertical diplopia with the findings of a 4th nerve palsy on the 3-step-test. What in addition to an acquired 4th nerve palsy, restriction, myasthenia, Wernicke encephalopathy and cranial arteritis should be considered and what would help confirm this?
70. What are 3 findings characteristic of a congenital a decompensated congenital 4th nerve palsy?
71. What should one consider with a hypertropia not mapping to a 4th nerve palsy?
72. How can one differentiate a skew deviation from a 4th nerve palsy?
Teaching Video NeuroImages: Bilateral abducens ocular neuromyotonia
Teaching Video NeuroImages: Bilateral abducens ocular neuromyotonia
Kavin Vanikieti and Joseph F. Rizzo
Neurology September 05, 2017; 89 (10)
RESIDENT AND FELLOW SECTION http://n.neurology.org/content/89/10/e128
A 44-year-old woman with a history of resolved nasopharyngeal carcinoma presented with an 8-month history of transient binocular horizontal diplopia. She received complete concurrent chemoradiotherapy 7 years ago. Following prolonged eccentric gaze to the right, she developed involuntary contraction of right lateral rectus, which resulted in 60 seconds of right exotropia. These events also occurred following prolonged eccentric gaze to the left, which resulted in left exotropia (video 1). Treatment with carbamazepine improved her symptoms (video 2). Ocular neuromyotonia should be included as a differential diagnosis of transient diplopia, especially in those who have undergone prior radiotherapy to the parasellar region.1
Video 1 – Pretreatment
Following prolonged eccentric gaze to the right, the patient developed involuntary contraction of right lateral rectus, which resulted in right exotropia. Each episode lasted approximately 60 seconds and then the eyes returned to normal alignment. These events also occurred following prolonged eccentric gaze to the left, which resulted in left exotropia.
Video 2 – Post Treatment
Complete resolution with carbamazepine
Teaching Slides – PowerPoint Presentation
Reference: 1. Leigh RJ, Zee DS. The Neurology of Eye Movements, 5th ed. Oxford: Oxford University Press; 2015:615.
Questions of the week: NOI13 Diplopia 5 – 6th Nerve Palsy
NOI13 Diplopia 5 – 6th Nerve Palsy
Questions:
1. Where is the nucleus of the 6th cranial nerve located?
2. Which cranial nerve passes through theDorellocanal beneath the petroclynoid (Gruber) ligament?
3. What are the clinical findings of a unilateral 6th nerve nuclear lesion?
4. Why does a unilateral nuclear 6th nerve palsy cause an ipsilateral horizontal gaze palsy?
5. Why is a unilateral 6th nerve palsy often accompanied by an ipsilateral 7th nerve palsy?
6. Where does an ipsilateral Horner syndrome and 6th nerve palsy localize the lesion?
7. Where does an ipsilateral Horner syndrome and 6th nerve palsy associated with a third, fourth, V1 and V2 deficit localize?
8. A microvascular 6th nerve palsy is suspected because a 60-year-old patient has diabetes, hypertension and hyperlipidemia, what tests should be done?
9. A presumed microvascular 6th nerve palsy is suspected in a 60-year-old patient with diabetes, hypertension and hyperlipidemia has not resolved within 3-6 months, what test should be ordered?
10. What is Brown syndrome?
11. What explains the findings of Duane syndrome?
12. What are the findings of Duane syndrome?
13. Are systemic associations common in Duane syndrome?
14. What is the Möbius syndrome?
15.What should be done in a patient with bilateral 6th nerve palsies and a normal MRI?
16. What is best initial imaging study for an isolated 6th nerve palsy in 20-year-old?
17. What is the best initial treatment for a comitant small-angle 6th nerve palsy?
18. What is the likelihood that an isolated,vasculopathic6th nerve palsy will recover?
19. What condition does convergence spasm mimic?
20. What are the findings of convergence spasm?
21. What exam technique should be used in suspected bilateral or unilateral 6th nerve palsy to eliminate convergence spasm?
22. What may mimic a 6th nerve palsy?
Clinical Reasoning: A 22-year-old man with diplopia
Clinical Reasoning: A 22-year-old man with diplopia
Chelsea Meyer, DO, Don Raphael P. Wynn, MD, Stefan M. Pulst, MD, DrMed Ricky Chen, MD, Kathleen Digre, MD Correspondence to Dr. Meyer: chelsea.meyer@hsc.utah.edu
Neurology October 11, 2016; 87 (15)
RESIDENT & FELLOW SECTION Section Editor John J. Millichap, MD
SECTION 1
A 22-year-old previously healthy man presented to an ophthalmology clinic with binocular horizontal diplopia. He had recently traveled to the main island of Hawaii. About 2 weeks after returning home, he developed a severe headache with associated fever, emesis, photophobia, phonophobia, and neck stiffness. He also reported a sensation of pressure in his left eye and both ears but denied any pulsatile tinnitus or transient vision loss. Over the next 2 weeks, his headaches worsened, causing him to wake up frequently in the night. He then developed horizontal diplopia that was worse at a distance and was referred to the neuro-ophthalmology clinic. Examination. The patient had some limitation in neck flexion with associated pain. His visual acuity was 20/20 on the right and 20/25 on the left. Pupillary examination showed no relative afferent defect and visual fields were full. He was found to have bilateral abducens palsy with an esotropia of 30 D and a left hypertropia of 2 D with notable mild right head tilt. The hypertropia was thought to be a partial left 4th nerve palsy with a compensatory right head tilt, although a full Parks-Bielschowsky 3-step test was not preformed to confirm this. He had moderate to severe papilledema on funduscopic examination (figure, A). The remainder of his neurologic and ophthalmologic examination was within normal limits.
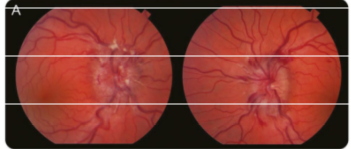
Figure (A) Funduscopic photographs of the optic disc of the left eye show papilledema with blurring of the disc margin, optic nerve hyperemia, and peripapillary hemorrhages.
Questions for consideration:
1. Given his papilledema and bilateral abducens nerve palsy, where would you localize this?
2. What is the differential diagnosis for bilateral abducens nerve palsy?