Questions:
1. Are some maculopathies associated with mild optic nerve pallor?
2. Can maculopathies have dyschromatopsia?
3. In evaluating optic neuritis, when should a lumbar puncture for CSF analysis be considered?
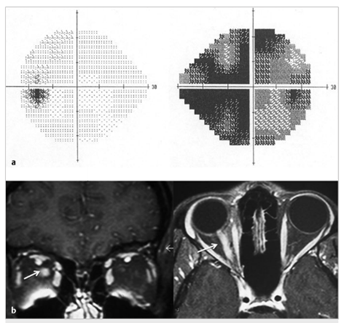
Fig.8.5
(a) Isolated right inflammatory optic neuropathy. There is a large central scotoma seen as diffuse depression on a 24–2 Humphrey visual field test.
(b)Coronal and axial T1-weighted magnetic resonance imaging with fat suppression and contrast showing enhancement of the orbital portion of the right optic nerve(arrow).
 Fig.8.1
Fig.8.1 1
1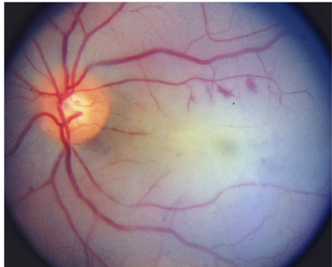 1
1