Teaching NeuroImages: Upright-supine test to evaluate vertical diplopia
Nailyn Rasool and Sashank Prasad
Neurology May 12, 2015; 84 (19)
RESIDENT AND FELLOW SECTION
Article:
A 36-year-old woman presented with vertical diplopia, nausea, and disequilibrium. Maddox rod testing was performed in the upright and supine positions (figures 1 and 2).
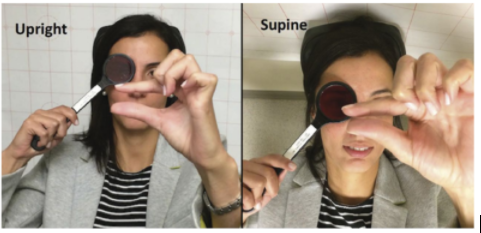
Figure 1 Upright-supine test
During Maddox rod testing, the patient used her fingers to demonstrate the separation of images.
The vertical deviation decreased substantially (over 50%) when supine compared to upright.