Questions:
16. What condition should be considered in any patient over 50 with transient or constant diplopia?
17. What condition should be considered in any patient over 50 with headaches
18. Is Cranial Arteritis common, uncommon, or rare among Blacks, Hispanics, Asians, and Whites?
19. What percent of patients will have premonitory visual symptoms, usually within the week preceding permanent visual loss from Cranial Arteritis?
20. What are the 7 ophthalmic signs in a patient with anterior ischemic optic neuropathy that are highly suggestive of Cranial Arteritis?
21. In what percentage of patients with Cranial Arteritis will the ESR be normal?
22. Is the CRP ever normal in Cranial Arteritis?
23. What other blood tests may be elevated in Cranial Arteritis?
24. How long will patients with Cranial Arteritis generally need to be treated with oral steroids?
25. At what rate should oral prednisone be tapered in Cranial Arteritis?
26. What test is the only test that confirms the diagnosis of temporal arteritis?
Neuro-ophthalmology Illustrated Chapter 20 – Conditions Commonly Encountered in Neuro-ophthalmology 2
Neuro-ophthalmology Question of the Week: Neuro-ophthalmology Coma Eye Exam
Question:
Which of the following are correct for a patient?
1. The eyes of a patient in coma will be closed.
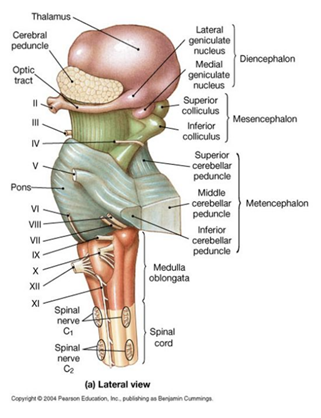
2. Because the pathways governing ocular motility traverse the entire brainstem, brainstem lesions will most often result in abnormal eye movements, and the lesion can be localized to the midbrain, pons, or medulla.
3. The presence of a dysconjugate ocular deviation in coma (horizontal, vertical, or oblique misalignment) often indicates a cranial nerve palsy or skew deviation.
4. Roving eye movements: slow ocular conjugate deviations in random directions indicate intact ocular motility function in the brainstem.
5. Periodic alternating (“ping-pong”) gaze: slow, repetitive, rhythmic, back-and-forth, horizontal conjugate eye movements indicates intact ocular motility function in the brainstem.
6. Normal vertical and horizontal oculocephalic reflexes indicate intact ocular motility function in the brainstem.
 1
1
Neuro-ophthalmology Question of the Week: Emergency Department Evaluation of Anisocoria
 1
1
Question:
Describe the appropriate steps to take in the emergency department when evaluating anisocoria.
Neuro-ophthalmology Question of the Week: Emergency Department Evaluation of Ptosis
 4
4
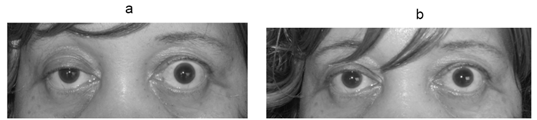
a. Photograph of the patient showing right partial ptosis. The left lid shows compensatory lid retraction because of equal innervation of the levator palpabrae superioris (Herring’s law).
b. Post tensilon test: Note the improvement in ptosis.
Question: Describe the appropriate steps to take in the emergency department when evaluating ptosis of recent onset.
Neuro-ophthalmology Question of the Week: Emergency Department Evaluation of Bilateral Disc Edema
Question: Describe the appropriate steps to take in the emergency department when evaluating bilaterally swollen discs.
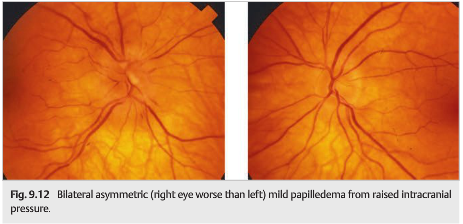 3
3
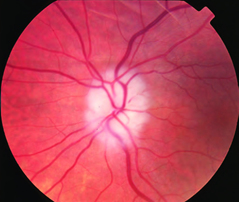
Neuro-ophthalmology Question of the Week: Emergency Department Evaluation of Monocular Sustained Vision Loss
Question: Describe the appropriate steps to take in evaluating sustained monocular vision loss in the emergency department.
 6
6
Neuro-ophthalmology Question of the Week: Emergency Department Evaluation of Binocular Transient Vision Loss
Question: Describe the appropriate steps to take in evaluating binocular transient vision loss (BTVL) in the emergency department.
Neuro-ophthalmology Question of the Week: Emergency Department Evaluation of Monocular Transient Vision Loss
Question: Describe the appropriate steps to take in evaluating monocular transient vision loss (TVL) in the emergency department.
Neuro-ophthalmology Question of the Week: Neuro-ophthalmic Emergencies

Question: Identify 7 symptoms or examination findings that are often associated with pathology that require immediate assessment to enable potential life and/or vision saving emergent therapy?