NOI13 Diplopia 6 – 4th Nerve Palsy
Questions:
63. What are 6 characteristics of a 4th nerve palsy?
64. When a patient has a 3rd nerve palsy and the eye cannot adduct, how can the function of the ipsilateral 4th nerve shown to be present?
65. What other conditions should be considered when the patient has the findings of a 4th nerve palsy?
66. A patient has a 4th nerve lesion associated with a contralateral Horner syndrome, where does this localize the lesion?
67. A microvascular 4th nerve palsy is suspected because a 60-year-old patient has diabetes, hypertension and hyperlipidemia what should be ordered?
68. A presumed microvascular 4th nerve palsy in a 60-year-old patient with diabetes, hypertension and hyperlipidemia has not resolved within 3-6 months, what test should be ordered?
69. A 60 year-old patient presents with intermittent vertical diplopia with the findings of a 4th nerve palsy on the 3-step-test. What in addition to an acquired 4th nerve palsy, restriction, myasthenia, Wernicke encephalopathy and cranial arteritis should be considered and what would help confirm this?
70. What are 3 findings characteristic of a congenital a decompensated congenital 4th nerve palsy?
71. What should one consider with a hypertropia not mapping to a 4th nerve palsy?
72. How can one differentiate a skew deviation from a 4th nerve palsy?
____________________________________________________
Questions with answers:
63. What are 6 characteristics of a 4th nerve palsy?
1. Binocular vertical/oblique diplopia.
2. An ipsilateral hypertropia.
3. Difficulty looking down when the eye is adducted.
4. The hypertropia is greater when they look to the opposite side.
5. The hypertropia is greater when they tilt their head toward the same side.
6. They spontaneously tilt their head to the contralateral side to compensate for their diplopia.
64. When a patient has a 3rd nerve palsy and the eye cannot adduct, how can the function of the ipsilateral 4th nerve shown to be present?
To check that the fourth nerve functions normally when there is a third cranial nerve palsy, check that intorsion of the eye is preserved, a function that is best seen in abduction.
1. Ask the patient to abduct the eye with the third nerve palsy.
2. Once the eye is in abduction, ask the patient to look down, and look carefully for intorsion by focusing on a scleral/conjunctival vessel.
3. Intact intorsion confirms that the fourth nerve is functional.
65. What other conditions should be considered when the patient has the findings of a 4th nerve palsy?
Not all patients with an apparent superior oblique weakness have a 4th nerve palsy. Consider restriction of the muscle, skew deviation, myasthenia, Wernicke encephalopathy and if over age 50, cranial arteritis.
66. A patient has a 4th nerve lesion associated with a contralateral Horner syndrome, where does this localize the lesion?
The lesion localizes to the 4th nerve nucleus on the same side as the Horner syndrome.
67. A microvascular 4th nerve palsy is suspected because a 60-year-old patient has diabetes, hypertension and hyperlipidemia what should be ordered?
Microvascular 4th nerve palsies are most often nonarteritic, but giant cell arteritis should always be considered and CBC, platelets, ESR and CRP should be ordered. The patient should be observed for spontaneous recovery for 3-6 months. Neuroimaging – MRI Brain with and without contrast to rule-out a mass lesion should also be done if follow-up is not reliable.
68. A presumed microvascular 4th nerve palsy in a 60-year-old patient with diabetes, hypertension and hyperlipidemia has not resolved within 3-6 months, what test should be ordered?
Neuroimaging – MRI Brain with and without contrast to rule-out a mass lesion if not done initially.
69. A 60 year-old patient presents with intermittent vertical diplopia with the findings of a 4th nerve palsy on the 3-step-test. What in addition to an acquired 4th nerve palsy, restriction, myasthenia, Wernicke encephalopathy and cranial arteritis should be considered?
Decompensating congenital 4th nerve palsy.
70. What are 3 findings characteristic of a congenital a decompensated congenital 4th nerve palsy?
A decompensated congenital 4th nerve palsy usually has:
1. A longstanding head tilt usually obvious on old photographs.
2. Overaction of the ipsilateral inferior oblique in adduction.
3. A large vertical fusional amplitude of 10 to 15 prism diopters (normal vertical fusional amplitude is between 2 and 3 prism diopters).
71. What should one consider with a hypertropia not mapping to a 4th nerve palsy?
Skew deviation. Skew deviation is due to vestibular pathway dysfunction.
Possible companions: Nystagmus, INO, Impaired vestibulo-ocular reflex.
72. How can one differentiate a skew deviation from a 4th nerve palsy?
The upright-supine test helps differentiate a skew deviation from trochlear nerve palsy: a vertical deviation that decreases by ≥ 50% from the upright to supine position suggests a skew deviation. This is often done with a Maddox rod.
________________________________________________
The information below is from: Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
13.5.3 The Lesion Involves a Cranial Nerve
The diagnosis and management of ocular motor cranial nerve dysfunction vary according to the age of the patient, characteristics of the cranial nerve palsy, and presence of associated symptoms and signs.
Fourth Cranial Nerve (Trochlear Nerve) Palsies
Patients with a fourth nerve palsy have a superior oblique weakness. A fourth nerve palsy results in difficulty looking down when the eye is positioned in toward the nose.
Patients complain of binocular vertical (or oblique) diplopia, especially when going down the stairs and reading. They have an ipsilateral hypertropia that is worse when they look to the other side and worse when they tilt their head toward the same side. They spontaneously tilt their head to the contralateral side to compensate for their diplopia.
Right superior oblique paresis (▶Fig. 13.79) has the following characteristics:
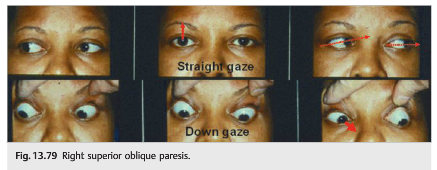
● Decreased depression
● Right hypertropia
● Hypertropia worsens in left gaze
● Worse with right head tilt
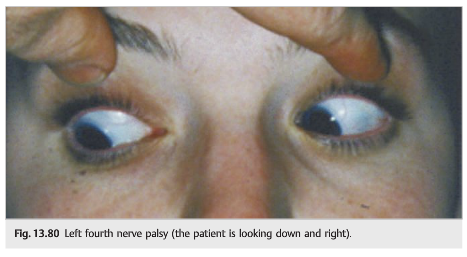
A fourth nerve palsy also results in decreased intorsion, and some patients mention that one image is tilted (▶Fig. 13.80).
When there is also a third nerve palsy, the eye cannot adduct (▶Fig. 13.81).
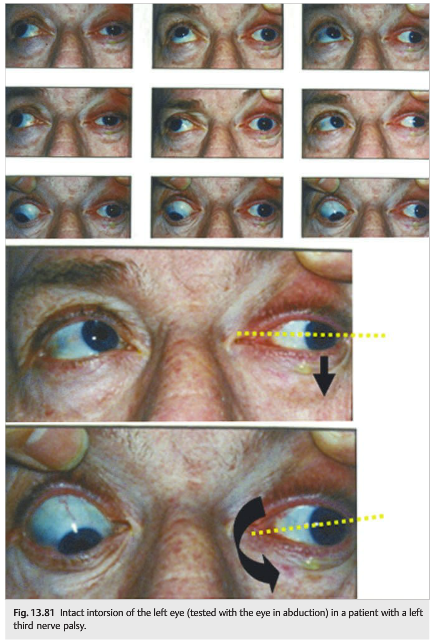
To check that the fourth nerve functions normally when there is a third cranial nerve palsy, check that intorsion of the eye is preserved, a function that is best seen in abduction.
1. Ask the patient to abduct the eye with the third nerve palsy (left eye in this example).
2. Once the eye is in abduction, ask the patient to look down, and look carefully for intorsion by focusing on a scleral vessel.
3. Intact intorsion confirms that the fourth nerve is functional.
Pearls
Not all patients with a superior oblique paresis have a fourth nerve palsy (disorders of the muscle and myasthenia can also give a superior oblique weakness). Fourth nerve palsies may be difficult to differentiate from skew deviation.
The upright-supine test helps differentiate a skew deviation from trochlear nerve palsy: a vertical deviation that decreases by ≥ 50% from the upright to supine position suggests a skew deviation.
Anatomy of the Fourth Cranial Nerve (▶Fig. 13.82)
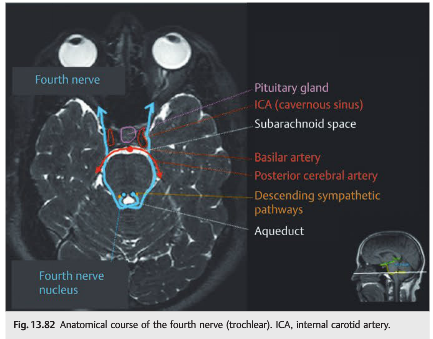
The fourth nerve is unique in its dorsal exit from the midbrain, posterior crossover within the subarachnoid space, and innervation of the superior oblique muscle contralateral to its nucleus. Because of these anatomical features and the resultant long course from midbrain to muscle, the fourth nerve is particularly vulnerable to injury in the setting of head trauma.
● The nucleus is located at the ventral border of the periaqueductal gray matter, at the level of the inferior colliculus, and lies immediately next to the descending sympathetic pathways.
● The fascicle exits posteriorly and crosses over to the contralateral side of the midbrain.
● The nerve travels ventrally within the subarachnoid space (longest intracranial course of all cranial nerves, measuring 75mm).
● It then curves around the upper pons where it passes between the superior cerebellar artery and the posterior cerebral artery to reach the prepontine cistern.
● The nerve then enters the lateral wall of the cavernous sinus and lies below the third nerve and above the ophthalmic division of the fifth nerve (V1).
● It reaches the orbital apex.
● The nerve enters the superior orbit outside of the annulus of Zinn to innervate the superior oblique muscle.
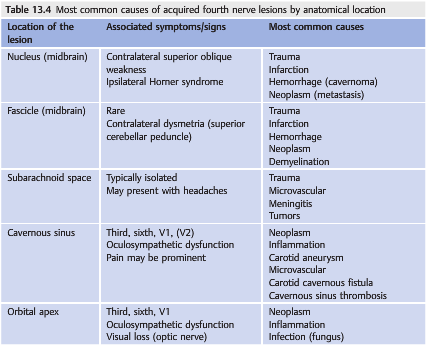
Causes of Fourth Cranial Nerve Palsies (▶Table 13.4)
● A fourth nerve nuclear lesion causes a superior oblique palsy clinically similar to a fourth nerve lesion. However, the superior oblique weakness is contralateral to the nuclear lesion because of the fourth nerve’s decussation after its dorsal emergence from the midbrain.
● A fourth nerve nuclear lesion is often associated with a Horner syndrome because the descending sympathetic pathway is very close to the fourth nerve nucleus (the Horner syndrome is on the side of the nuclear lesion, whereas the superior oblique paresis will involve the opposite eye).
● The two most common causes of fourth nerve palsy are trauma (unilateral or bilateral fourth nerve palsy) and decompensation of a congenital fourth nerve palsy.
● An isolated fourth nerve palsy occurring in a patient older than 50 and with atheromatous vascular risk factors is often a microvascular fourth nerve palsy. Mild brow pain is common. The fourth nerve palsy almost always resolves completely within 3 to 6 months. Rarely, a microvascular fourth nerve palsy may be arteritic, related to vasculitis (especially giant cell arteritis).
Pearls
● Microvascular fourth nerve palsies are most often nonarteritic, but giant cell arteritis should always be considered.
● A microvascular fourth nerve palsy should resolve within 3 to 6 months.
●Persistent deficit should prompt imaging, if not performed initially.
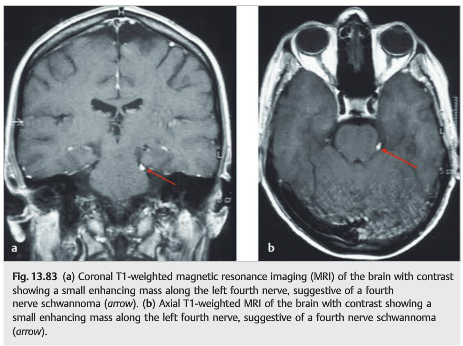
Rarely, an isolated fourth nerve palsy is secondary to a small tumor of the nerve in the subarachnoid space. In most cases, these tumors are schwannomas. Their prognosis is good, and symptomatic treatment of diplopia, such as prisms or even strabismus surgery if stable ocular deviation, is offered (▶Fig. 13.83).
Congenital Fourth Cranial Nerve Palsy
Congenital fourth cranial nerve palsy is common and may decompensate at any age.
● Decompensated congenital fourth nerve palsy presents as intermittent diplopia in a patient with a long-standing head tilt (obvious on old photographs).
● There is evidence of chronicity as shown by the following:
○ Overaction of the ipsilateral inferior oblique in adduction (the eye shoots up in adduction)
○ Large vertical fusional amplitude, up to 10 or 15 prism diopters (patient’s ability to fuse vertically separated images despite the placement of progressively larger amounts of vertical prism over one eye; normal vertical fusional amplitude is between 2 and 3 prism diopters) (▶Fig. 13.84)

Causes of Fourth Cranial Nerve Palsies in Children
Fourth nerve palsies are less common in children than sixth and third nerve palsies.
Trauma represents the most common cause.
Congenital fourth nerve palsies are often not diagnosed in childhood.
Evaluation of the Patient with Suspected Fourth Cranial Nerve Palsy
● Based on other illnesses and age
● Neurological evaluation looking for other symptoms or signs
● Ophthalmological evaluation looking for orbital syndrome, optic neuropathy, papilledema, other ocular motor cranial nerve involvement
● Systemic evaluation looking for giant cell arteritis (if over 50), fever, systemic inflammatory disorder, atheromatous vascular risk factors
● Could it be myasthenia?
● Is the fourth nerve palsy isolated, or not?
● Is the fourth nerve palsy painful, or not?
● Is the fourth nerve palsy chronic?
○ Review old photos for head tilt.
○ Look for inferior oblique overaction.
○ Look for large vertical fusion amplitude.
Patients with isolated fourth nerve palsy need to be evaluated as follows:
● If post-traumatic or decompensation of congenital fourth nerve palsy, no further workup
● Patient older than 50 years: CBC, platelets, CRP, ESR, glucose, lipid profile
● If acquired and no precipitating trauma
○ MRI brain and orbits with fat suppression and gadolinium with special attention to the course of the fourth nerve: midbrain, cavernous sinus, pituitary gland, orbital apex, and orbit (trochlea)
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections totcooper@stanford.edu.