Questions:
1. What is the difference in the meaning of functional, nonphysiologic, and nonorganic visual loss?
2. What is the only way to confirm the diagnosis of nonorganic visual loss?
3. Is it common for nonorganic symptoms to be superimposed on organic disease?
4. In a patient complaining of substantial visual loss in only one eye, and no history of amblyopia and a normal standard eye examination, what 4 tests that can be used to determine if the vision loss is inorganic?
5. What are 2 techniques for the Fogging test for functional vision loss?
6. How is the horizontal prism shift test performed?
7. How is the vertical prism dissociation test performed?
8. When the complaint is “No Light Perception or Hand Motion Vision in Both Eyes”, what 5 tests that can be used to determine if that the vision loss is inorganic?
9. What visual field findings are common in nonorganic visual loss?
Neuro-ophthalmology Illustrated Chapter 18 – Nonorganic Neuro-ophthalmologic Signs and Symptoms 1
Recommended Reading – The expanding burden of idiopathic intracranial hypertension
Recommended Reading – The expanding burden of idiopathic intracranial hypertension
The expanding burden of idiopathic intracranial hypertension
Susan P. Mollan, Magda Aguiar, Felicity Evison, Emma Frew & Alexandra J. Sinclair. Eye (2018)
Free Full Text: https://www.nature.com/articles/s41433-018-0238-5
Abstract
OBJECTIVE: To quantify the hospital burden and health economic impact of idiopathic intracranial hypertension.
METHODS: Hospital Episode Statistics (HES) national data was extracted between 1st January 2002 and 31st December 2016. All those within England with a diagnosis of idiopathic intracranial hypertension were included. Those with secondary causes of raised intracranial pressure such as tumours, hydrocephalus and cerebral venous sinus thrombosis were excluded.
RESULTS: A total of 23,182 new IIH cases were diagnosed. Fifty-two percent resided in the most socially deprived areas (quintiles 1 and 2). Incidence rose between 2002 and 2016 from 2.3 to 4.7 per 100,000 in the general population. Peak incidence occurred in females aged 25 (15.2 per 100,000). 91.6% were treated medically, 7.6% had a cerebrospinal fluid diversion procedure, 0.7% underwent bariatric surgery and 0.1% had optic nerve sheath fenestration. Elective caesarean sections rates were significantly higher in IIH (16%) compared to the general population (9%), p < 0.005. Admission rates rose by 442% between 2002 and 2014, with 38% having repeated admissions in the year following diagnosis. Duration of hospital admission was 2.7 days (8.8 days for those having CSF diversion procedures). Costs rose from £9.2 to £50 million per annum over the study period with costs forecasts of £462 million per annum by 2030.
CONCLUSIONS: IIH incidence is rising (by greater than 100% over the study), highest in areas of social deprivation and mirroring obesity trends. Readmissions rates are high and growing yearly. The escalating population and financial burden of IIH has wide reaching implications for the health care system.
Composite figure.
a Incidence in the general population. b Incidence by age and gender. c Annual incidence in females and males and Obesity rates (% obesity per annum (body mass index ≥ 30), age-standardized in 18 years + by gender in the United Kingdom. From World Health organisation http://apps.who.int/gho/data/node.main.A900A?lang=en Accessed 6 Oct 2017. d Management of IIH in the cohort. e Geographical distribution of diagnosed cases of IIH in England. F Distribution of cases by region per annum.
Neuro-ophthalmology questions of the week: NOI20- Conditions Commonly Encountered in Neuro-ophthalmology 2
Questions:
14. In which type of patient is Cranial Arteritis common, uncommon and rare – Blacks, Hispanics or Whites?
15. What condition should be considered in any patient over 50 with headaches?
16. What condition should be considered in any patient over 50 with transient or constant diplopia?
17. What percent of patients will have premonitory visual symptoms, usually within the week preceding permanent visual loss from Cranial Arteritis?
18. Name the 7 ophthalmic signs that with AION suggest a high risk for Cranial Arteritis?
19. In what percentage of patients with Cranial Arteritis will the ESR be normal?
20. Is the CRP ever normal in Cranial Arteritis?
21. What other blood tests may be elevated in Cranial Arteritis?
22. How long will patients with Cranial Arteritis generally need to be treated with oral steroids?
23. At what rate should oral prednisone be tapered in Cranial Arteritis?
24. What test is the only test that confirms the diagnosis of temporal arteritis?
Neuro-ophthalmology Questions of the Week-Neuroretinitis
Questions:
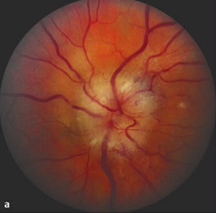
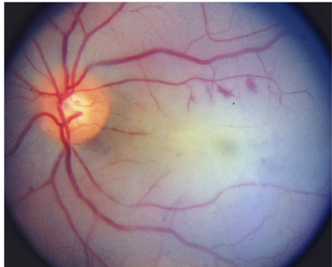
1. What are the ophthalmoscopic characteristics of neuroretinitis?
2. Is neuroretinitis caused by demyelination?
3. In what settings does neuroretinitis most commonly occur?
 1
1
Neuro-ophthalmology Question of the Week-Acute Disseminated Encephalomyelitis (ADEM)
Questions:
1. Is ADEM more common in in children or adults?
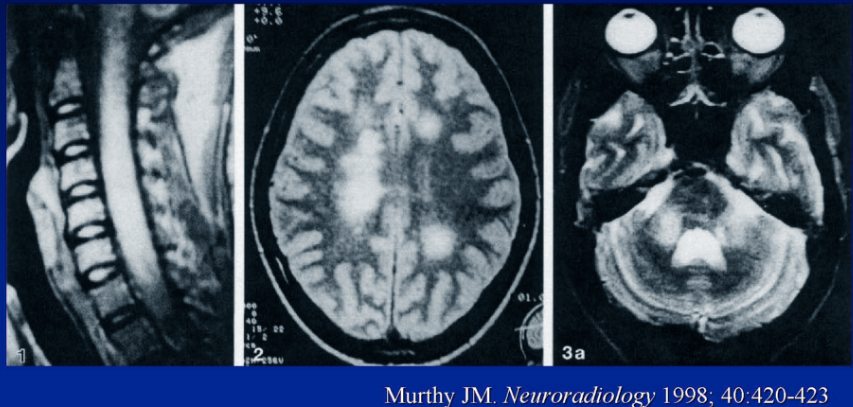
2. What may the clinical symptoms and MRI changes of ADEM mimic?
3. How many symptomatic episodes of ADEM is a patient likely to experience?
4. Is optic neuritis seen in some patients with ADEM?
 1
1
Neuro-ophthalmology Questions of the Week-Ocular Vascular Disease
Questions:
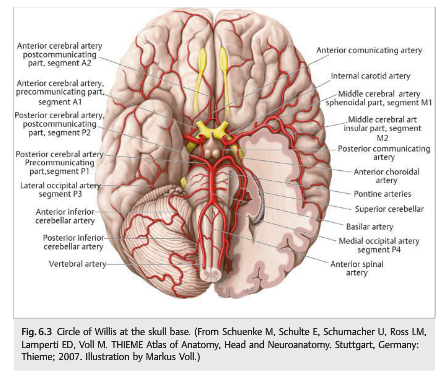
- What may develop in patients with severe stenosis or occlusion of the ipsilateral common carotid artery or internal carotid artery and poor collateral circulation?
- What condition should venous stasis retinopathy, or hypotensive retinopathy, suggest?
- What are the symptoms of the ocular ischemic syndrome?
- What are signs of the ocular ischemic syndrome?
- What is the prognosis of the ocular ischemic syndrome?
- What should be ruled-out in a patient who has a rapidly worsening ocular ischemic syndrome?
- What should be checked in all patients with headache and bilateral optic nerve swelling?
- What 10 classic systemic disorders are associated with retinal vasculitis?
- Is radiation retinopathy a chronic, painless, progressive retinal vasculopathy?
- Radiation retinopathy may be unilateral or bilateral and occur months or years after radiotherapy. True or False?
- Radiation retinopathy is more common in patients with underlying retinal vascular disease (e.g., hypertension or diabetes). True or False?
- What are 5 key findings of radiation retinopathy?
- What are 6 Complications of radiation retinopathy?
- What is the chief feature of Purtscher retinopathy?
- What is the significance of bilateral retinal vascular tortuosity?
- What are 2 retinal vascular malformations?
 1
1
Neuro-ophthalmology Questions of the Week-Retinal Ischemia
Questions:
1. What should be done for a patient with monocular vision loss, not due to nonarteritic anterior ischemic optic neuropathy, arteritic anterior ischemic optic neuropathy, or other ophthalmologic disease, but with branch or central retinal artery occlusions or amaurosis fugax?
2. What should be considered if a central artery is associated with pain?
3. What is the most common cause of ophthalmic artery occlusion?
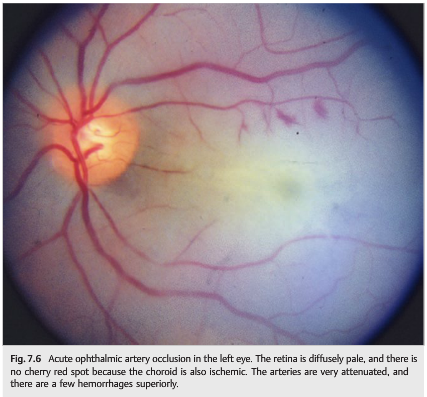
4. What are the findings from ophthalmic artery occlusion
5. What finding seen in acute central artery occlusion is not seen with acute ophthalmic artery occlusion?
6. What work-up should be done when retinal emboli are found in an asymptomatic patient?
7. What is the appearance of cholesterol emboli?
8. What are common sources for cholesterol emboli?
9. What is the appearance of talc emboli?
10. What condition is associated with talc emboli?
11. In a patient with acute retinal ischemia what tests should be ordered for thrombophilia?
 1
1
Neuro-ophthalmology Question of the Week-Binocular Transient Visual Loss
Question: What are 5 categories of symptoms that help differentiate the 3 most common causes of binocular transient vision loss (migraine visual aura, occipital transient ischemic attacks, and occipital seizures)?
 1
1
Neuro-ophthalmology Questions of the Week-Vascular Transient Monocular Visual Loss
Questions:
1. What should be done immediately when a patient presents with a recent vascular TMVL?
2. What should be done emergently in the presence of an acute central retinal artery or branch retinal artery occlusion?
3. What is the chance and timeline of stroke after TMVL in the presence of ipsilateral atheromatous internal carotid stenosis ≥50%?
4. What is the yearly risk of vascular death (myocardial infarction) in patients with TMVL and atheromatous disease?
 1
1
Neuro-ophthalmology Question of the Week: Transient Monocular Vision Loss Categories
Neuro-ophthalmology Question of the Week: Transient Monocular Vision Loss Categories
Question: What are the three main categories of transient monocular vision loss?
 1
1