Questions:
10. What should 2 conditions should be suspected in a patient with binocular diplopia, marked esotropia, and an apparent bilateral gaze palsy?
11. What are the findings of convergence spasm?
12. In a patient with binocular horizontal diplopia, marked esotropia, and an apparent bilateral gaze palsy what exam 4 techniques can be used to rule-out convergence spasm?
13. What are 3 characteristics of voluntary nystagmus?
14. What is the visual complaint of patients with voluntary nystagmus?
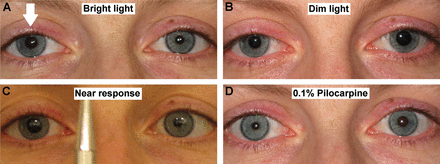
15. What pharmacologic agents should be used to rule-out pharmacologic mydriasis in a patient with a fixed dilated pupil?
16. Will mydriasis from a 3rd nerve palsy constrict to 0.1% pilocarpine?
17. If a pupil constricts with 0.1% pilocarpine what condition is present?
18. Will mydriasis from a 3rd nerve palsy constrict to 1% pilocarpine?
19. Will a pupil with pharmacologic mydriasis fully constrict to 1% pilocarpine?
20. A patient with best corrected distance visual acuity of 20/20, is unable to read better than J10 at near. What test can determine if the cause is inorganic?
21. How can nonorganic unilateral ptosis be differentiated from organic ptosis?
22. How can nonorganic blepharospasm be treated?
23. After it has been established that the patient’s symptoms are functional, what approach to treatment should be taken?
Neuro-ophthalmology Illustrated Chapter 18 – Nonorganic Neuro-ophthalmologic Signs and Symptoms 2
Neuro-ophthalmology Illustrated Chapter 1 – Examination 3
Questions:
11. Which 5 features of pupil function should be documented in a neuro-ophthalmic examination?
12. Would a Relative Afferent Pupillary Defect be expected with anisocoria?
13. Does an occipital lobe injury result in a Relative Afferent Pupillary Defect?
14. Does a unilateral optic neuropathy result in a Relative Afferent Pupillary Defect?
15. Can a unilateral optic tract lesion result in a Relative Afferent Pupillary Defect?
16. What anatomic factor explains the Relative Afferent Pupillary Defect with an optic tract lesion?
Neuro-ophthalmology Questions of the Week: Other Pupillary Abnormalities
Questions:
1. What is a tadpole pupil?
2. What are 6 causes of light-near dissociation?
3. Where is the lesion in a patient with light-near dissociation due to Argyll Robertson pupils?
4. What is the mechanism of light-near dissociation due to Argyll Robertson pupils?
5. Where is the lesion in a patient with light-near dissociation due to Adie tonic pupil?
6. What is the mechanism of light-near dissociation due to Adie tonic pupil?
7. What is the mechanism of light-near dissociation due to aberrant regeneration of the 3rd nerve?
8. What is the mechanism of light-near dissociation due to severe vision loss?
9. What is the mechanism of light-near dissociation due to laser panretinal photocoagulation or cryotherapy?
10. Where is the lesion in a patient with light-near dissociation due to peripheral neuropathy?
11. What are paradoxical pupillary reactions?
12. What is spasm of convergence?
 1
1
Neuro-ophthalmology Questions of the Week: Pupil – Abnormal Mydriasis
Questions:
1. What are ocular disorders that keep a large pupil from constricting?
2. How does one test for pharmacologic mydriasis from topical agents?
3. What are two conditions that cause mydriasis via the parasympathetics?
4. What are the clinical symptoms and signs of Adie tonic pupil
5. What explains the light-near dissociation classically found in Adie tonic pupil syndrome.
6. What topical drop is used to confirm the presence of Adie pupil syndrome?
7. What may happen to the size of the pupil over time in the Adie syndrome?
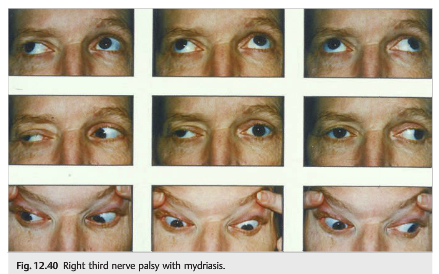
8. Is isolated mydriasis likely to be caused by a 3rd nerve paresis?
9. Is complete mydriasis likely to be related to a 3rd nerve paresis?
10. Do all 3rd nerve paresis have pupillary involvement?
11. What diagnoses should we worry about for a patient with an isolated third nerve palsy with mydriasis?
 1
1
Neuro-ophthalmology Questions of the Week: Pupil – Abnormal Miosis
Questions:
1. What are the signs of Horner Syndrome?
2. What signs and symptoms and signs can be associated with Horner syndrome?
3. Which eye drops can be used to establish the diagnosis of Horner syndrome?
4. What is the mechanism of action of cocaine when used to test Horner syndrome?
5. What is observed when testing for Horner syndrome with cocaine?
6. What is the mechanism of action of the apraclonidine when used to test Horner syndrome?
7. What is observed when testing for Horner syndrome with apraclonidine?
8. Which eye drop is used to localize which order neuron is involved in Horner syndrome?
9. What is the mechanism of hydroxyamphetamine when used to test Horner syndrome?
10. What is observed when hydroxyamphetamine is used to test Horner syndrome?
11. What is the classic cause of a first-order neuron Horner syndrome?
12. What does the combination of an ipsilateral Horner syndrome (first-order) and contralateral superior oblique palsy (fourth nerve palsy) suggest?
13. What does the combination of an ipsilateral Horner syndrome and (third-order) and an abducens paresis suggest?
14. What should the presumed cause of an acute painful Horner syndrome?
15. If the localization of a Horner syndrome is unknown what imaging tests should be done?
16. In a young child with an isolated Horner syndrome a workup should be done for what condition?
17. What imaging test should be done in a child with a Horner syndrome without a surgical history to explain it?
Neuro-ophthalmology Questions of the Week: Pupils – Anisocoria
Questions:
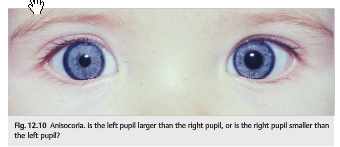
1. What specific steps should be followed in examining a patient with anisocoria?
2. What are the characteristics of physiologic anisocoria?
3. What are the ocular causes of anisocoria?
Neuro-ophthalmology Questions of the Week: Pupils – Examination, Anatomy & Physiology
Questions:
1. When examining the pupils, what should you record?
2. Does a RAPD cause anisocoria?
3. If a patient is suspected of having optic neuropathy (regardless of the cause) has no RAPD does that rule-out this diagnosis?
4. If a patient has a severe bilateral optic neuropathy will the pupils respond to near stimuli?
5. Which order neuron is involved when the Horner syndrome is caused by a tumor in the apex of a lung?
6. Why do patients with a third-order Horner syndrome usually do not have anhidrosis?
7. What is neurotransmitter is released at the neuromuscular junction of the iris sphincter to result in pupillary constriction?
8. What is neurotransmitter is released at the neuromuscular junction of the iris sphincter to result in pupillary dilation?
9. Why do lesions of the geniculate nucleus, the optic radiations, or the visual cortex not affect pupillary size or pupillary reactivity?
10. What is the course of the parasympathetic fibers for pupillary constriction from the Edinger-Westphal nucleus to the ciliary ganglion?
11. What is the ratio of postganglionic parasympathetic fibers that innervate the ciliary muscle to those that innervate the pupillary sphincter muscle?

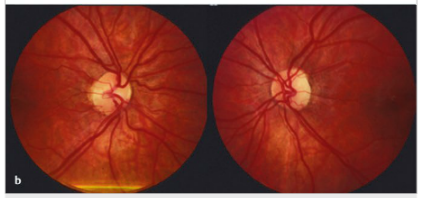
Neuro-ophthalmology Question of the Week: Optic Tract Defects
Question:
Which of the following are correct for a left optic tract lesion?
1. Right homonymous hemianopia
2. Left RAPD
3. Bowtie atrophy of the right optic nerve
4. Mostly temporal pallor of the left optic nerve
 1
1
Neuro-ophthalmology Question of the Week: Dilated pupil constricts to pilocarpine 0.125%
Question1:
A 35-year-old woman is evaluated for a 2-week history of photophobia and awareness that her right pupil is larger than the left. Examination shows absent right pupillary response to light stimulation of either eye. There is no diplopia and no evidence of extraocular muscle palsy. Upon local instillation of 0.125% pilocarpine, the larger pupil becomes smaller than the contralateral pupil.
Which of the following is the most likely location of the lesion?
1. ciliary ganglion
2. Edinger-Westphal nucleus
3. oculomotor nerve
4. optic chiasm
5. pretectal nucleus
 2
2
Neuro-ophthalmology Question of the Week: Anisocoria – Horner syndrome & Heterochromia Iridis
Question: Which of the following are correct?
1. A heterochromia iridis-associated acquired Horner syndrome is usually due to a lesion of the postganglionic neuron (third order).
2. Heterochromia iridis-associated acquired Horner syndrome only occurs in children?
3. In a patient with isolated heterochromia iridis-associated Horner syndrome, the lighter eye is the one with the oculosympathetic paresis.
4. When both Waardenburg and congenital Horner syndromes occur in the same individual the darker iris is the one with the oculosympathetic paresis.
 1
1