Questions:
8. What tests should be done in all patients over age 50 with transient or permanent diplopia?
9. What is the Silent Sinus Syndrome?
10. What is the Kearns-Sayre syndrome?
11. What are 5 mitochondrial diseases that can have ophthalmoplegia?
12. What are the features of Myotonic Dystrophy?
13. What are the features of Oculopharyngeal Dystrophy?
14. What 3 conditions other than paresis or restriction should be considered in any adult with new-onset transient or permanent ocular misalignment?
15. What may induce the myasthenia gravis or make it worse?
16. What is the mechanism of action of edrophonium?
17. What are the side effects of the Tensilon test?
18. What does the development of lid retraction in a patient with Myasthenia suggest?
19. What percent of patients presenting with purely ocular myasthenia will progress to develop generalized disease?
20. Does myasthenia gravis ever affect the pupils?
21. Does myasthenia gravis ever cause pain?
Archives for 2018
Questions of the Week: Diplopia 4 – Binocular Diplopia 2
Clinical Reasoning: A 20-year-old man with headache and double vision
Khaled Moussawi, Anoopum Gupta and Haatem Reda
Neurology October 11, 2016; 87 (15)
Correspondence to Dr. Moussawi: khaled.moussawi@nih.gov
RESIDENT AND FELLOW SECTION
Section Editor John J. Millichap, MD
From Harvard Medical School (K.M., A.G., H.R.), Boston; Department of Neurology (K.M., A.G., H.R.), Massachusetts General Hospital, Boston; and Department of Neurology (K.M., A.G.), Brigham and Women’s Hospital, Boston, MA. Dr. Moussawi is currently with the National Institute on Drug Abuse; and the Department of Psychiatry, Johns Hopkins Medicine, Baltimore, MD.
SECTION 1
A 20-year-old man presented to the emergency department with 1 week of headaches and double vision following 2 days of fever (1028 F), nausea, and vomiting. His headache was progressively worsening, throbbing behind his right eye, nonpositional, and associated with photophobia, blurry vision, and pain with eye movement. Occasionally, it was severe enough to wake him up from sleep. Horizontal double vision ensued soon after the headache. His diplopia was worse looking at a distance, improved on leftward gaze, worsened on rightward gaze, and resolved with closing one eye. He denied neck stiffness, focal weakness, numbness, or other neurologic symptoms. He denied recent rashes, infections, or tick bites. He lives on a farm in central Brazil. He arrived in Massachusetts 2 months before his presentation to visit family members. He had no significant medical history and took no medications. He did not smoke or use drugs.
Question for consideration:
1. What is the localization of his presenting symptom?
Questions of the Week: Diplopia 3 Diagnosis of Binocular Diplopia 1
Questions:
1. What is the most common cause of unilateral proptosis?
2. What is the most common cause of bilateral proptosis?
3. Which is the most commonly involved extraocular muscle in thyroid eye disease?
4. What conditions should be considered in a patient with enlarged extraocular muscles?
5. On CT or MRI, which condition spares the insertions of the extraocular muscles, thyroid eye disease or idiopathic orbital inflammation (orbital pseudotumor)?
6. What 4 features differentiate idiopathic orbital inflammation (orbital pseudotumor) from thyroid eye disease?
7. When should a biopsy be done in a patient with presumed “myositis”?
Clinical Reasoning: Two see or not two see—Is it really double vision?
Clinical Reasoning: Two see or not two see—Is it really double vision?
Richard Ronan Murphy, MBChB Abdullah Al Sawaf, MD Danny R. Rose Jr., MD Larry B. Goldstein, MD Charles D. Smith, MD
Neurology August 08, 2017; 89 (6)
RESIDENT AND FELLOW SECTION
RESIDENT & FELLOW SECTION
Section Editor John J. Millichap, MD
Correspondence to R.R. Murphy: ronan.murphy@uky.edu
SECTION 1
A 57-year-old right-handed woman presented to the emergency department with complaints of double vision and intractable nausea that began abruptly 2 days earlier. Her visual symptoms were characterized as seeing overlapping or separate horizontally or diagonally displaced objects. She had no history of headaches or stroke. Her cerebrovascular risk factors included hypertension, type II diabetes, coronary artery disease, and cigarette smoking. Her medications included clopidogrel, lisinopril, paroxetine, and oxycodone. Her family history was notable for late-onset ischemic heart disease in her parents with no first-degree relatives with early vascular disease. On examination, her blood pressure was 158/101 mm Hg, pulse rate was 87 bpm, and she was afebrile. She was alert and fully oriented. Her attention, recall of recent events, and general fund of knowledge were normal. Her speech was fluent and nondysarthric. Cranial nerve examination was notable for no dysconjugacy or nystagmus, but double vision predominately in the horizontal plane, in all directions of gaze. The diplopia persisted with monocular vision in each eye, and did not improve with a pinhole test. The degree of diplopia waxed and waned during the examination, with visual field extinction tests being difficult to perform reliably. Her pupils were equal with bilateral hippus. Visual fields were full to confrontation. Direct funduscopy revealed normal optic discs. She had a mild right hemiparesis with mild right arm and leg drift, but no facial asymmetry. There was mild hypesthesia over her right arm and leg and appendicular ataxia in her right arm that was worse with eyes open. She did not have extinction to double simultaneous sensory stimuli. Gait evaluation was deferred during her initial examination.
Questions for consideration:
1. What is the significance of the presence of diplopia in both eyes, with either eye closed?
2. What more could be elicited from the history and examination to help characterize the problem?
Questions of the Week: Diplopia 2 – Assessment
Questions:
13. How is Bell phenomenon checked in normal patients?
14. When Bell’s phenomenon is preserved despite an upgaze paresis, where is the lesion?
15. What is the localizing value of abnormal eye movements that are overcome by oculocephalic maneuvers?
16. What is the usual symptom noted by a patient with convergence insufficiency?
17. A patient presents with a history of the onset of diplopia 3 weeks ago. What should be the first characteristic of the diplopia determined?
18. Your exam confirms that a patient has patient binocular diplopia, but on exam the extraocular movements appear full. What must be present?
19. Your exam confirms that a patient has patient binocular diplopia, but on exam the extraocular movements appear full. What tests will be helpful in demonstrating the misalignment?
20. What will the cross-cover test detect that the cover-uncover test will not detect?
21. When is a phoria pathologic and not physiologic?
22. Is the 3-step-test useful in horizontal or vertical binocular diplopia?
23. What reflex is involved in the 3rd step of the 3-step-test?
24. With the red Maddox rod placed between placed between a light source and the eye, what does the eye see?
25. Why would one perform a double Maddox Rod test?
26. When are the Hirschberg and Krimsky tests useful?
27. How is the Hirschberg test performed?
28. How is the Krimsky test performed?
29. In a comatose patient you observe dysconjugate horizontal eye movements when the head is rotated from side to side. What does this suggest?
Heimann-Bielschowsky phenomenon
Recommended Reading
Teaching Video NeuroImages: Heimann-Bielschowsky phenomenon
A harmless monocular nystagmus
Article:
Heimann-Bielschowsky phenomenon (HBP) is a rare form of dissociated nystagmus.1 A 38-year-old man complained of poor vision in his right eye for 6 years. Right visual acuity was 20/200 due to traumatic aphakia (cataract extraction without intraocular lens) and 20/20 in the left eye. An asymptomatic coarse, low frequency, pendular, vertical nystagmus was manifest in the right eye only (video, http://links.lww.com/WNL/A177). HBP is an asymptomatic monocular slow, pendular, mostly vertical nystagmus, which can develop years after uniocular severe visual loss.1 The pathogenesis of HBP is debated, but vertical fusion disruption due to monocular visual loss is hypothesized.2 Recognizing HBP should prevent unnecessary investigations or treatments.
Teaching slides: http://links.lww.com/WNL/A178
Video: http://links.lww.com/WNL/A177
Neurology
February 20, 2018; 90 (8)
RESIDENT & FELLOW SECTION
References
- Yee RD, Jelks GW, Baloh RW, Honrubia V. Uniocular nystagmus in monocular visual loss. Ophthalmology 1979;86:511–522.
- Leigh RJ, Thurston SE, Tomsak RL, Grossman GE, Lanska DJ. Effect of monocular visual loss upon stability of gaze. Invest Ophthalmol Vis Sci 1989;30:288–292.
Neuro-ophthalmology Questions of the Week: Diplopia1 – Basics
Questions:
1. What 5 anatomical components of eye movement can cause binocular diplopia?
2. What holds the image steady during brief head movements?
3. What holds the image steady during sustained head movements?
4. What is Sherrington’s law?
5. What is Hering’s Law?
6. What 2 processes cause most incomitant strabismus?
7. What is the primary deviation in incomitant strabismus?
8. What is the secondary deviation in incomitant strabismus?
9. In incomitant strabismus, is the primary or secondary deviation larger?
10. Does a phoria or a tropia have more value in localizing the defect in a patient with new onset binocular diplopia
11. What is the difference between terms “ocular motor” and “oculomotor”?
12. What is the difference between ductions, versions and vergences?
13. What 3 techniques can help determine if an ocular misalignment is due to a restriction or paresis?
Neuro-ophthalmology Questions of the Week: Other Pupillary Abnormalities
Questions:
1. What is a tadpole pupil?
2. What are 6 causes of light-near dissociation?
3. Where is the lesion in a patient with light-near dissociation due to Argyll Robertson pupils?
4. What is the mechanism of light-near dissociation due to Argyll Robertson pupils?
5. Where is the lesion in a patient with light-near dissociation due to Adie tonic pupil?
6. What is the mechanism of light-near dissociation due to Adie tonic pupil?
7. What is the mechanism of light-near dissociation due to aberrant regeneration of the 3rd nerve?
8. What is the mechanism of light-near dissociation due to severe vision loss?
9. What is the mechanism of light-near dissociation due to laser panretinal photocoagulation or cryotherapy?
10. Where is the lesion in a patient with light-near dissociation due to peripheral neuropathy?
11. What are paradoxical pupillary reactions?
12. What is spasm of convergence?
 1
1
Neuro-ophthalmology Questions of the Week: Pupil – Abnormal Mydriasis
Questions:
1. What are ocular disorders that keep a large pupil from constricting?
2. How does one test for pharmacologic mydriasis from topical agents?
3. What are two conditions that cause mydriasis via the parasympathetics?
4. What are the clinical symptoms and signs of Adie tonic pupil
5. What explains the light-near dissociation classically found in Adie tonic pupil syndrome.
6. What topical drop is used to confirm the presence of Adie pupil syndrome?
7. What may happen to the size of the pupil over time in the Adie syndrome?
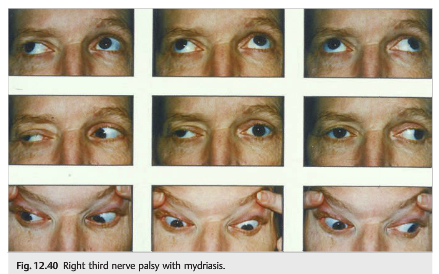
8. Is isolated mydriasis likely to be caused by a 3rd nerve paresis?
9. Is complete mydriasis likely to be related to a 3rd nerve paresis?
10. Do all 3rd nerve paresis have pupillary involvement?
11. What diagnoses should we worry about for a patient with an isolated third nerve palsy with mydriasis?
 1
1
Neuro-ophthalmology Questions of the Week: Pupil – Abnormal Miosis
Questions:
1. What are the signs of Horner Syndrome?
2. What signs and symptoms and signs can be associated with Horner syndrome?
3. Which eye drops can be used to establish the diagnosis of Horner syndrome?
4. What is the mechanism of action of cocaine when used to test Horner syndrome?
5. What is observed when testing for Horner syndrome with cocaine?
6. What is the mechanism of action of the apraclonidine when used to test Horner syndrome?
7. What is observed when testing for Horner syndrome with apraclonidine?
8. Which eye drop is used to localize which order neuron is involved in Horner syndrome?
9. What is the mechanism of hydroxyamphetamine when used to test Horner syndrome?
10. What is observed when hydroxyamphetamine is used to test Horner syndrome?
11. What is the classic cause of a first-order neuron Horner syndrome?
12. What does the combination of an ipsilateral Horner syndrome (first-order) and contralateral superior oblique palsy (fourth nerve palsy) suggest?
13. What does the combination of an ipsilateral Horner syndrome and (third-order) and an abducens paresis suggest?
14. What should the presumed cause of an acute painful Horner syndrome?
15. If the localization of a Horner syndrome is unknown what imaging tests should be done?
16. In a young child with an isolated Horner syndrome a workup should be done for what condition?
17. What imaging test should be done in a child with a Horner syndrome without a surgical history to explain it?