Questions:
1. What are the signs of Horner Syndrome?
2. What signs and symptoms and signs can be associated with Horner syndrome?
3. Which eye drops can be used to establish the diagnosis of Horner syndrome?
4. What is the mechanism of action of cocaine when used to test Horner syndrome?
5. What is observed when testing for Horner syndrome with cocaine?
6. What is the mechanism of action of the apraclonidine when used to test Horner syndrome?
7. What is observed when testing for Horner syndrome with apraclonidine?
8. Which eye drop is used to localize which order neuron is involved in Horner syndrome?
9. What is the mechanism of hydroxyamphetamine when used to test Horner syndrome?
10. What is observed when hydroxyamphetamine is used to test Horner syndrome?
11. What is the classic cause of a first-order neuron Horner syndrome?
12. What does the combination of an ipsilateral Horner syndrome (first-order) and contralateral superior oblique palsy (fourth nerve palsy) suggest?
13. What does the combination of an ipsilateral Horner syndrome and (third-order) and an abducens paresis suggest?
14. What should the presumed cause of an acute painful Horner syndrome?
15. If the localization of a Horner syndrome is unknown what imaging tests should be done?
16. In a young child with an isolated Horner syndrome a workup should be done for what condition?
17. What imaging test should be done in a child with a Horner syndrome without a surgical history to explain it?
____________________________________________________
Questions with answers:
1. What are the signs of Horner Syndrome?
● Reduced palpebral fissure: mild ptosis involving both upper and lower lids due to paralysis of the Müller muscles innervated by the sympathetic pathway
● Pseudo enophthalmos because of the reduced palpebral fissure
● Unilateral miosis
● Dilation lag in the dark (slow dilation of the affected pupil)
2. What signs and symptoms and signs can be associated with Horner syndrome?
● Anhidrosis of the ipsilateral face in preganglionic lesions (first- or second-order Horner syndrome)
● Brainstem and spinal cord symptoms and signs suggestive of a first-order Horner Syndrome
● Arm pain, hand weakness, and history of neck surgery or neck trauma suggestive of a second-order Horner syndrome
● Ipsilateral facial pain suggestive of a third-order Horner syndrome
3. Which eye drops can be used to establish the diagnosis of Horner syndrome?
Cocaine drops are used but are difficult to obtain. Apraclonidine drops are now replacing cocaine for the diagnosis of Horner syndrome.
4. What is the mechanism of action of cocaine when used to test Horner syndrome?
Cocaine blocks the reuptake of norepinephrine at the sympathetic nerve synapse with the iris dilator.
5. What is observed when testing for Horner syndrome with cocaine?
It causes pupillary dilation in eyes with intact sympathetic innervation and has no effect in eyes with impaired sympathetic innervation, regardless of the lesion location (little or no norepinephrine is being released into the synaptic cleft tonically).
6. What is the mechanism of action of the apraclonidine when used to test Horner syndrome?
Apraclonidine is a direct alpha-receptor agonist (strong alpha-2 and weak alpha-1).
7. What is observed when testing for Horner syndrome with apraclonidine?
It has no effect in eyes with intact sympathetic innervation and causes mild pupillary dilation in eyes with sympathetic denervation, regardless of the lesion location (with denervation hypersensitivity, alpha-1 effect dilates the Horner pupil and elevates the ptotic lid). Apraclonidine reverses the Horner syndrome.
8. Which eye drop is used to localize which order neuron is involved in Horner syndrome?
Hydroxyamphetamine
9. What is the mechanism of hydroxyamphetamine when used to test Horner syndrome?
Hydroxyamphetamine releases stored norepinephrine from the postganglionic adrenergic nerve endings.
10. What is observed when hydroxyamphetamine is used to test Horner syndrome?
It causes pupillary dilation in eyes with intact sympathetic innervation or intact postganglionic fibers and has no or partial effect in eyes with impaired sympathetic innervation from lesions involving the postganglionic fibers (no effect on third-order Horner syndrome).
11. What is the classic cause of a first-order neuron Horner syndrome?
It is ipsilateral a medullary infarction (Wallenberg syndrome); other causes are ipsilateral various thalamic, brainstem, and spinal cord lesions.
12. What does the combination of an ipsilateral Horner syndrome (first-order) and contralateral superior oblique palsy (fourth nerve palsy) suggest?
It suggests a lesion of the trochlear nucleus or its fascicle in the brainstem.
13. What does the combination of an ipsilateral Horner syndrome and (third-order) and an abducens paresis suggest?
The combination of an ipsilateral Horner syndrome (third-order) and an abducens paresis suggests a lesion in the cavernous sinus.
14. What should an acute painful Horner syndrome be presumed to be due to?
An acute painful Horner syndrome should be presumed related to a dissection of the ipsilateral internal carotid artery unless proven otherwise. These patients are at risk of cerebral infarction and should be evaluated emergently.
15. If the localization of a Horner syndrome is unknown what imaging tests should be done?
If localization is unknown, image brain, neck, spinal cord, carotid arteries, and pulmonary apex (may require multiple imaging tests). The easiest test is a CT/CTA of the head, neck, and chest allows good examination of the brain and spine, of the soft tissues, and of large blood vessels in the head, neck, and chest as well as examination of the pulmonary apex. A MRI/MRA of this area is an alternative.
16. In a young child with an isolated Horner syndrome a workup should be done for what condition?
Neuroblastoma
17. What imaging test should be done in a child with a Horner syndrome without a surgical history to explain it?
To rule out a neuroblastoma, order an MRI scan of the head, neck, and chest with contrast; an MRI scan of the abdomen if there is high clinical suspicion; and tests for urinary catecholamines (vanillylmandelic acid [VMA] and homovanillic acid [HVA]). MRA scans of the neck and aortic arch are also often obtained.
Explanation:
“Miosis (the Small Pupil Is Abnormal)
Miosis, or excessive smallness or contraction of one pupil, is diagnosed when the small pupil does not dilate as well as the large pupil in dim light.
Miosis can be related to an ocular condition that keeps the small pupil from dilating (e.g., uveitis, previous ocular surgery, or pseudoexfoliation syndrome) or to pharmacologic constriction of the pupil (by drops, e.g., pilocarpine). Brimonidine tartrate (used topically to treat glaucoma) usually decreases the pupil size. This effect is not noticeable when patients place drops in both eyes, but it can induce anisocoria when used to treat unilateral glaucoma.
When the ocular and pharmacologic causes are excluded, pupillary miosis usually results from dysfunction of the ipsilateral sympathetic pathway, or Horner Syndrome.
Horner Syndrome (Oculosympathetic Paresis)
Features and Diagnosis
The signs of Horner syndrome include the following (▶Fig. 12.22):
● Reduced palpebral fissure: mild ptosis involving both upper and lower lids due to paralysis of the Müller muscles innervated by the sympathetic pathway
● Pseudo Enophthalmos because of the reduced palpebral fissure
● Unilateral miosis
● Dilation lag in the dark (slow dilation of the affected pupil)

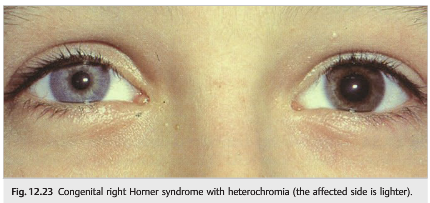
Heterochromia in congenital Horner syndrome (lighter color on affected side)(▶Fig. 12.23)
Associated neurologic symptoms and signs include the following:
● Anhidrosis of the ipsilateral face (loss of sweating) in preganglionic lesions (first- or second-order Horner syndrome)
● Brainstem and spinal cord symptoms and signs suggestive of a first-order Horner Syndrome
● Arm pain, hand weakness, and history of neck surgery or neck trauma suggestive of a second-order Horner syndrome
● Ipsilateral facial pain suggestive of a third-order Horner syndrome
Pharmacologic testing confirms the diagnosis of Horner syndrome.
Cocaine drops are used but are difficult to obtain. Apraclonidine drops are now replacing cocaine for the diagnosis of Horner syndrome (apraclonidine is routinely used for glaucoma and is easy to obtain). The diagnosis of Horner syndrome with cocaine or apraclonidine can be performed in children, but apraclonidine should be avoided in young children less than 1 year of age (the punctum lacrima should be occluded with a finger while placing the drops to limit systemic effects in all children and in pregnant women).
Testing with cocaine involves the following:
1. Instill two drops of 4 or 10% cocaine in both eyes.
2. After 45 minutes to 1 hour,
● the normal pupil dilates,
● the Horner pupil dilates poorly, and
● anisocoria increases.
Cocaine blocks the reuptake of norepinephrine at the sympathetic nerve synapse with the iris dilator. It causes pupillary dilation in eyes with intact sympathetic innervation and has no effect in eyes with impaired sympathetic innervation, regardless of the lesion location (little or no norepinephrine is being released into the synaptic cleft tonically).
To test with apraclonidine (Iopidine):
1. Instill two drops of 0.5 or 1.0% apraclonidine in both eyes.
2. After 30 to 45 minutes,
● the normal pupil does not dilate,
● the Horner pupil dilates,
● anisocoria reverses, and
● the palpebral fissure enlarges on the side of the Horner syndrome.
Apraclonidine is a direct alpha-receptor agonist (strong alpha-2 and weak alpha-1). It has no effect in eyes with intact sympathetic innervation and causes mild pupillary dilation in eyes with sympathetic denervation, regardless of the lesion location (with denervation hypersensitivity, alpha-1 effect dilates the Horner pupil and elevates the ptotic lid). Apraclonidine reverses the Horner syndrome.
Localization
Horner syndrome is caused by a lesion anywhere along the sympathetic pathway that supplies the head, eye, and neck. Associated symptoms and signs usually allow localization of the lesion.
Pharmacologic testing helps localize the lesion along the sympathetic pathway (hydroxyamphetamine test). Except for rare emergencies, pharmacologic localization of the lesion should ideally be performed before obtaining any neuroimaging in adults. It is usually not performed in young children in whom the test is poorly reliable.
Testing with hydroxyamphetamine involves the following:
1. Instill two drops of 1% hydroxyamphetamine in both eyes.
2. After 45 minutes,
● the normal pupil dilates, and
● the Horner pupil dilates poorly if the lesion is postganglionic (third order), or
● the Horner pupil dilates if the lesion is preganglionic (first or second order).
Hydroxyamphetamine releases stored norepinephrine from the postganglionic adrenergic nerve endings. It causes pupillary dilation in eyes with intact sympathetic innervation or intact postganglionic fibers and has no or partial effect in eyes with impaired sympathetic innervation from lesions involving the postganglionic fibers (no effect on third-order Horner syndrome).
Because cocaine may interfere with the uptake and efficacy of hydroxyamphetamine drops, it is recommended that at least 72 hours elapse between the two tests. This is why the diagnosis of Horner syndrome is most often made clinically and only the hydroxyamphetamine test is performed to localize the lesion prior to obtaining a directed workup.
Horner Syndrome in Adults
The evaluation of an adult with Horner syndrome is mostly based on lesion location.
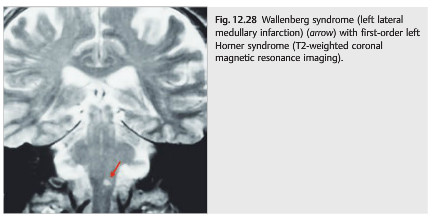
The most classic cause of a first-order Horner syndrome is ipsilateral medullary infarction (Wallenberg syndrome); other causes are ipsilateral various thalamic, brainstem, and spinal cord lesions (▶Fig. 12.28).
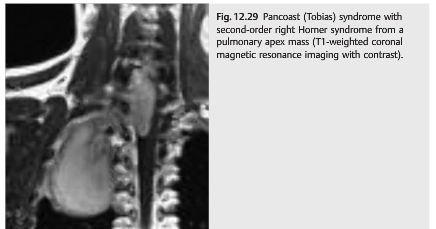
Second-order Horner syndromes are most suggestive of neoplasm or trauma of the lower cervical spine, brachial plexus, or lung apex (▶Fig. 12.29).
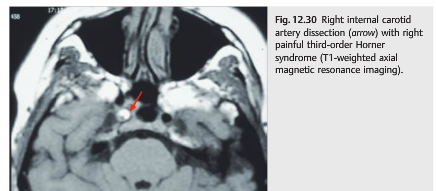
Third-order Horner syndromes point to lesions of the internal carotid artery, such as dissection and cavernous sinus aneurysms (▶Fig. 12.30).
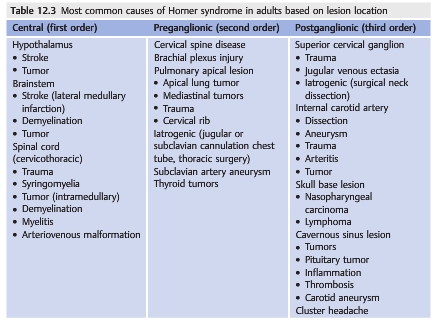
▶Table 12.3 summarizes the causes of Horner syndrome in adults.
Pearls
1. The combination of an ipsilateral Horner syndrome (first-order) and contralateral superior oblique palsy (fourth nerve palsy) suggests a lesion of the trochlear nucleus or its fascicle in the brainstem.
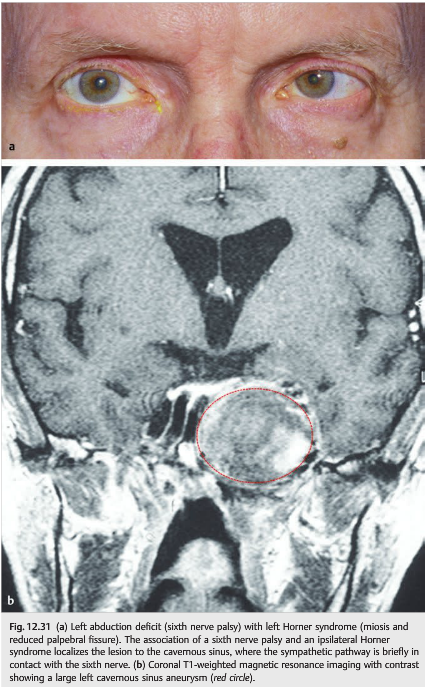
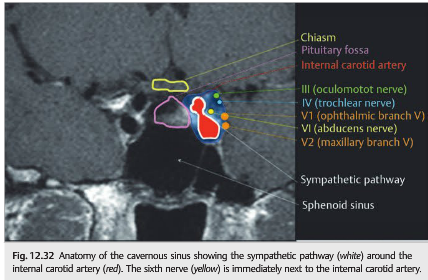
2. The combination of an ipsilateral Horner syndrome (third-order) and an abducens paresis (sixth nerve palsy) suggests a lesion in the cavernous sinus (▶Fig. 12.31 and ▶Fig. 12.32).
3. An acute painful Horner syndrome should be presumed related to a dissection of the ipsilateral internal carotid artery unless proven otherwise. These patients are at risk of cerebral infarction and should be evaluated emergently.
In evaluating an adult with isolated Horner syndrome, ask about the duration of symptoms, the presence of pain, and other symptoms or signs. Next, determine the localization of the lesion to the first-order, second-order, or third-order neuron. Finally, conduct a physical examination (ocular, neurologic, neck, supraclavicular, and chest).
The tests ordered will vary depending on the lesion location, the presence of associated symptoms or signs, the urgency of the workup, and the radiologist’s preference.
● For first- or second-order Horner syndrome, tests would include a chest X-ray, computed tomography (CT) or magnetic resonance imaging (MRI) of the chest (to view the pulmonary apex), and MRI with contrast of the head and neck. Magnetic Resonance angiography (MRA) of the aortic arch or computed tomographic angiography (CTA) of the head and neck may be required.
● For third-order Horner syndrome, tests would include MRI with contrast of the head and MRA or CTA of the head and neck.
● If localization is unknown, image brain, neck, spinal cord, carotid arteries, and pulmonary apex (may require multiple imaging tests). The easiest test is a CT/CTA of the head, neck, and chest allows good examination of the brain and spine, of the soft tissues, and of large blood vessels in the head, neck, and chest as well as examination of the pulmonary apex.
Horner Syndrome in Infants and Children
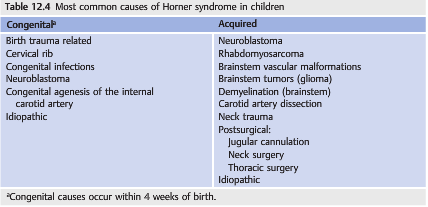
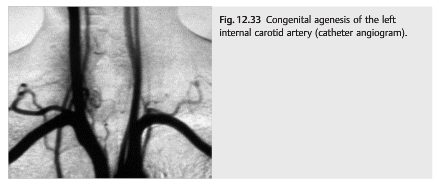
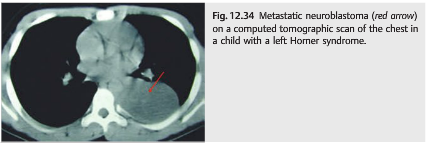
The etiology of Horner syndrome in infants and children differs from that for the adult population. The classic causes include birth trauma, neuroblastoma, vascular anomalies of the large arteries, and chest surgery (▶Table 12.4; ▶Fig. 12.33 and ▶Fig. 12.34).
Pearls
An isolated Horner syndrome in a young child should prompt a workup for neuroblastoma.
In evaluating a young child with isolated Horner syndrome, first determine any history of birth trauma, then conduct a physical examination, checking for a supraclavicular or abdominal mass. To rule out a neuroblastoma, order an MRI scan of the head, neck, and chest with contrast; an MRI scan of the abdomen if there is high clinical suspicion; and tests for urinary catecholamines (vanillylmandelic acid [VMA] and homovanillic acid [HVA]). MRA scans of the neck and aortic arch are also often obtained.
MRI of the head, neck, and chest as well as MRA of the head and aortic arch can be performed in one test under sedation in a young child. MRI of the abdomen usually requires a separate test (and therefore another sedation) and is often not required in a child with isolated Horner and normal abdominal examination.
Treatment of Horner Syndrome
Most patients with Horner syndrome have no visual changes and tolerate a mild ptosis. Rarely, lid surgery is requested to correct a persistent ptosis. Topical apraclonidine temporarily (a few hours) corrects the ptosis associated with Horner syndrome and may be used intermittently for cosmetic reasons or when the ptosis reduces the superior visual field.”1
Reference: 1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.