Question: When bilateral lesions of the retrochiasmal visual pathways produce a decrease in visual acuity which of the following are correct?
1. Such lesions produce symmetric VA loss in both eyes.
2. The VA loss from such lesions will be worse on the opposite side of the largest lesion.
3. The VA loss from such lesions will be worse on the same side of the largest lesion.
4. With the presence of retrochiasmal visual pathway lesions and different VA in the two eyes, an additional problem anterior to the chiasm must be present.
 1
1
 1
1 1
1 1
1 1
1 1
1 2
2 1
1 1
1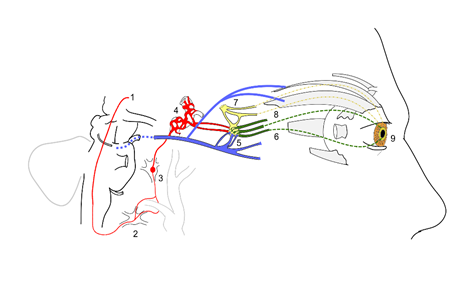 2
2