Question: Which of the following may reveal that the cause of anisocoria is not Horner syndrome?
1. Slit-lamp exam
2. The degree of anisocoria remains relatively constant in bright and dim illumination.
3. Repeat examinations of the patient on different days.
4. The absence of miosis on attempted near vision.
5. The failure of the pupil to constrict to light but does constrict with attempted near vision.
 2
2
_______________________________________
Correct Answers:
1. Slit-lamp exam
2. The degree of anisocoria remains relatively constant in bright and dim illumination.
3. Repeat examinations of the patient on different days.
Explanation:
Pseudo-Horner’s Syndrome and Simple Anisocoria1
Essential anisocoria Essential or physiologic anisocoria is a difference in pupillary size (generally less than 0.5 mm) that may be present in normal individuals. A pupil difference of 0.4 mm is easily noticeable, and 15% to 30% of the normal population may have at least this amount of anisocoria at any given time. In essential anisocoria, the pupillary inequality changes day to day and may even switch sides. This condition can usually be distinguished from pathologic states, as the degree of anisocoria remains relatively constant in light and dark.
Causes of anisocoria In addition to Horner’s syndrome, a miotic pupil can be the result of iridocyclitis, current or previous chronic use of miotic (glaucoma) eyedrops, Argyll Robertson pupil, old Adie’s pupil, and iris atrophy. It may be that the opposite, larger pupil is abnormal from trauma, pharmacologic agents, previous surgery, acute glaucoma, or other causes. Neovascularization of the iris and posterior synechia can cause a “stiff” pupil that can be larger or smaller that a normal pupil. Iris malformations and iris atrophy from any cause can also affect the size and function of the pupil [69]. Ophthalmologists may be in a position to avert an extensive neurologic evaluation by identifying iris structural abnormalities as the cause of anisocoria. [This is facilitated by the slit-lamp examination.]
Causes of ptosis/pseudoptosis
An idiopathic difference in palpebral fissure can be found in about 9% of normal individuals. Many disorders, other than Horner’s syndrome, can result in ptosis, including mechanical (from upper eyelid tumors, infiltration, edema, blepharochalasis), myogenic (myasthenia, chronic progressive external ophthalmoplegia), levator dehiscence (aging, trauma, inflammation, contact lens wear), and neurogenic (oculomotor nerve palsy) causes. Pseudoptosis can result from overhanging upper eyelid skin (dermatochalasis), relative enophthalmos (Duane’s syndrome, phthisis bulbi, microphthalmos, silent sinus syndrome [70]), overaction of eyelid protractors (blepharospasm, recovered facial nerve palsy), or eyelid retraction in the fellow eye (thyroid eye disease) [69].
Conclusions
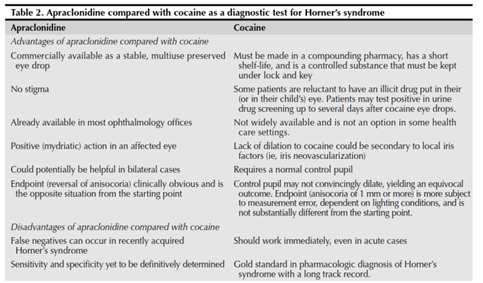
Since it was first recognized, Horner’s syndrome has been a frequent subject in the scientific literature. The recent case reports and series presented in this review should encourage the clinician to appreciate the diversity of disease process and anatomic location when evaluating patients with an oculosympathetic paresis. The experience to date regarding the diagnostic use of apraclonidine is quite positive, but the matter is not entirely settled. However, there is sufficient information to permit an informed clinician to use apraclonidine in the evaluation of patients with a suspected Horner’s syndrome (Fig. 2), especially in those cases when testing with cocaine is simply not an option. It is important to understand that all ocular pharmacologic tests should carry less weight than the clinical examination and the clinician’s suspicion. It is important for the clinician to understand the pharmacology of apraclonidine and other diagnostic agents, and thus understand their limitations and shortcomings. We are convinced that apraclonidine will remain an important tool in the diagnosis of Horner’s syndrome; however, future studies with greater numbers of subjects will tell us whether apraclonidine will unseat cocaine as the gold standard in the pharmacologic diagnosis of Horner’s syndrome.”1
 1
1
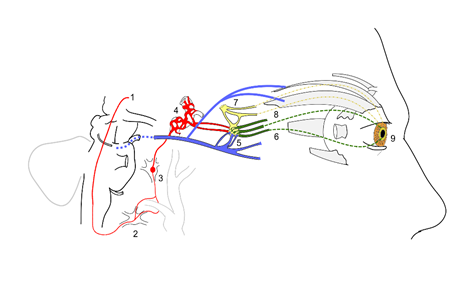
Autonomic innervation of the pupil and Horner’s syndrome diagram2
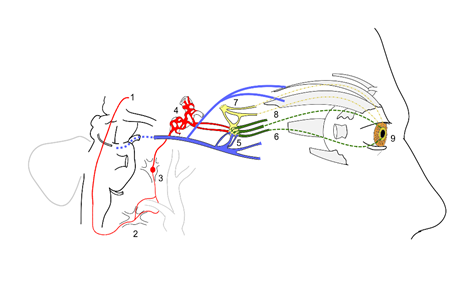
Sympathetic and parasympathetic innervation of the pupil and sites of lesion in a Horner’s syndrome.sympathetic fibers arise from the hypothalamus
- sympathetic fibers arise from the hypothalamus
- stellate ganglion
- synapse at the superior cervical ganglion
- sympathetic plexus around internal carotid artery
- oculomotor nerve (Cranial nerve 3) fibers synapse at the ciliary ganglion (blue)
- short ciliary nerves from ciliary ganglion carrying parasympathetic supply to sphincter pupillae (green)
- trigeminal fibers (Cranial nerve 5) relay in ciliary ganglion and carry sympathetic supply (yellow)
- long ciliary nerves (from the ophthalmic branch of CN 5) carrying sympathetic supply to the dilator pupillae
- dilator pupillae muscles of the pupil
Near the stellate ganglion, the sympathetic fibers go around the subclavian artery (shown along with the carotid vessels). This is a site of lesion especially due to its proximity to the apex of the lung (eg. Pancoast’s tumor).
The superior division of oculomotor nerve is shown supplying the Superior rectus and levator palpebrae superioris.
References:
- Horner’s syndrome, Pseudo-Horner’s syndrome, and simple anisocoria. Curr Neurol Neurosci Rep. 2007 Sep;7(5):397-406. Martin TJ.
- Autonomic innervation of the pupil and Horner’s syndrome. Suraj Rajan commons.wikimedia.org, http://commons.wikimedia.org/wiki/File:Horner%27s_Syndrome_and_Autonomic_innervation_of_the_eye.svg
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.