Neuro-ophthalmology Question of the Week: Optic Neuropathy or Maculopathy
Question:
Which of the following clinical tests can help differentiate between optic neuropathy and maculopathy in a patient with a reduction in visual acuity?
1.Swinging flashlight pupillary reactions
2. Amsler Grid
3. Dilation lag in darkness
4. Anisocoria
5. Photostress recovery test
6. Color vision/saturation
 1
1
_______________________________________________
Correct Answers:
1. Swinging flashlight pupillary reactions
2. Amsler Grid
3. Photostress recovery test
Explanation1:
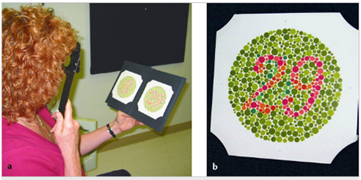
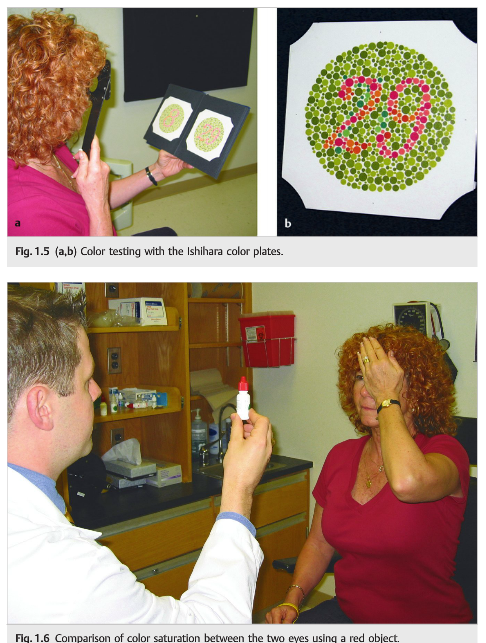
1.2 Color Vision, Color Saturation
Color vision can be assessed by several methods, and each eye is tested separately. The purpose of color vision testing is to detect acquired unilateral or bilateral color loss, which occurs most commonly with maculopathies, optic neuropathies, chiasmal disorders, and, more rarely, bilateral occipital lesions. The Ishihara pseudoisochromatic and the Hardy. Rand. Rittler (HRR) color plates are routinely used (Fig. 1. 5). The number of plates correctly identified with each eye is recorded (e. g. , “14/14 Ishihara color plates right eye; control only left eye”). The control plate can be read by patients with a visual acuity of at least 20/400. Some patients with dementia and simultagnosia may have difficulty using these plates. When color plates are unavailable, the difference in color perception between the two eyes may be identified using a red object (e. g. , the top from a bottle of dilating drops) (Fig. 1. 6). Even with normal color plate testing, the patient may recognize a color difference in a red bottle top alternately presented to each eye. The patient should be asked to quantify the red desaturation (percentage of normal).
1.4 Photostress Recovery Test
Photostress recovery is used to differentiate between macular disease and optic neuropathy. The principle underlying this test is that recovery of retinal sensitivity following exposure to a bright light is based on regeneration of visual pigments that were bleached during exposure to light. A delay in this process occurs in diseases affecting the photoreceptors and is independent of the neural pathways. Each eye is tested separately: 1. Measure the best corrected visual acuity in each eye. 2. Have the patient look directly into a bright light held a few centimeters from the eye for 10 seconds. 3. Record the time taken for the visual acuity to return to within one line of the best corrected visual acuity. Most normal patients will have a recovery time of less than 30 seconds, which is symmetric between the two eyes. Macular diseases (but not optic neuropathies) often cause a prolongation in the photostress recovery time. This is particularly useful for unilateral or subtle macular diseases.
1.5 Amsler Grid
The Amsler grid is very useful in detecting macular abnormalities as a cause of visual loss (Fig. 1. 7a). Each eye is tested separately, and the patient is asked to fixate on a central point in a square grid of lines and to draw any area in which the lines disappear or are broken,warped, double, or curved (Fig. 1. 7b). Patients with maculopathy often see the straight lines as curved (metamorphopsia).

1.9.1 Swinging Flashlight Test
A RAPD (Fig. 1. 17 and Fig. 1. 18) ipsilateral to visual loss indicates an optic neuropathy or severe retinal disease (in which case the retina looks abnormal on funduscopic examination). Ocular diseases, such as corneal abnormalities, cataracts, and most retinal disorders, do not cause RAPDs. Pathophysiology of the RAPD includes the following:1. When a light is directed into either eye, both pupils react equally. The brighter the light source, the greater the degree of bilateral pupillary constriction. 2. The amount of pupillary constriction from the same light source directed to either eye should be identical. 3. In unilateral optic nerve (or retinal ganglion cell) dysfunction, the light signal received by the brainstem efferent centers is relatively less than when the same light source is presented to the unaffected eye. Hence, both pupils constrict less when the involved eye is stimulated and more when the normal eye is stimulated. 4. A RAPD will not cause anisocoria.
A RAPD (Fig. 1. 17 and Fig. 1. 18) ipsilateral to visual loss indicates an optic neuropathy or severe retinal disease (in which case the retina looks abnormal on funduscopic examination). Ocular diseases, such as corneal abnormalities, cataracts, and most retinal disorders, do not cause RAPDs. Pathophysiology of the RAPD includes the following:1. When a light is directed into either eye, both pupils react equally. The brighter the light source, the greater the degree of bilateral pupillary constriction. 2. The amount of pupillary constriction from the same light source directed to either eye should be identical. 3. In unilateral optic nerve (or retinal ganglion cell) dysfunction, the light signal received by the brainstem efferent centers is relatively less than when the same light source is presented to the unaffected eye. Hence, both pupils constrict less when the involved eye is stimulated and more when the normal eye is stimulated. 4. A RAPD will not cause anisocoria.
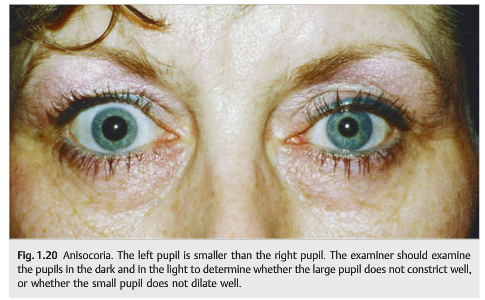
1.9.2 Anisocoria
Anisocoria (unequal pupils; Fig. 1. 20) means there is an abnormality of the efferent (sympathetic or parasympathetic) portion of the pupil pathways. Lesions of the afferent pathways do not produce anisocoria. When evaluating a patient with anisocoria, pupil examination in the dark and light allows determination of which pupil is abnormal.
Dilation Lag
Horner Syndrome (Oculosympathetic Paresis) Features and Diagnosis
The signs of Horner syndrome include the following (Fig. 12. 22):
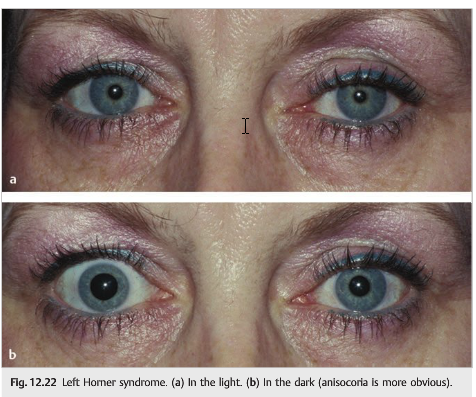
- Reduced palpebral fissure: mild ptosis involving both upper and lower lids due to paralysis of the Müller muscles innervated by the sympathetic pathway
- Pseudoenophthalmos because of the reduced palpebral fissure
- Unilateral miosis
- Dilation lag in the dark (slow dilation of the affected pupil)
Reference: 1. Neuro-ophthalmology Illustrated. 2nd Edition. Biousse V and Newman NJ. 2012. Theme
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz. com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology. stanford.edu
Follow https://twitter. com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.