Questions:
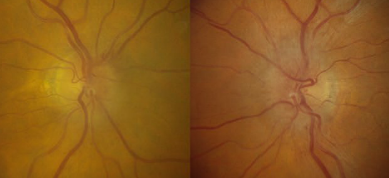
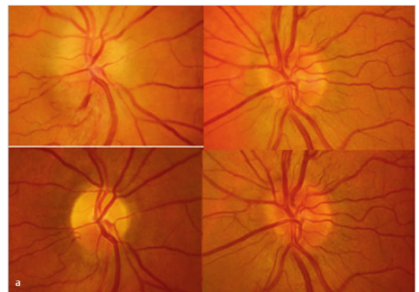
1. Are cases of toxic or nutritional optic neuropathies likely to be caused by a single agent?
2. Is vision likely to recover with discontinuation of the toxin or vitamin deficiency supplementation?
3. What are the common agents that cause toxic optic neuropathies?
4. What are the common agents that cause nutritional optic neuropathies?
5. What condition do the fundus findings of amiodarone toxicity often resemble?
6. What should always be checked in patients with progressive bilateral visual loss and bilateral optic atrophy?
 1
1
Neuro-ophthalmology Questions of the Week: Toxic and Nutritional Optic Neuropathies
Neuro-ophthalmology Questions of the Week: Compressive and Infiltrative Optic Neuropathies
Questions:
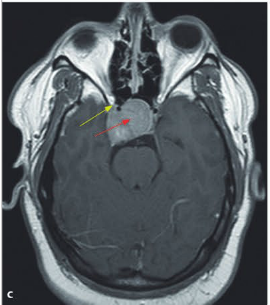
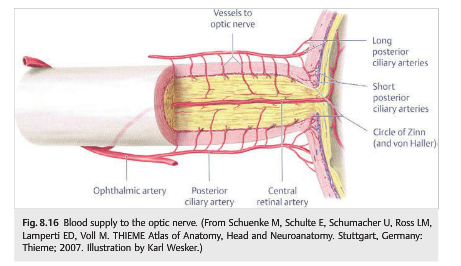
1. What is the most common cause of compressive optic neuropathy?
2. Are pilocytic astrocytoma and optic nerve glioma more common in adults or children?
3. Do anterior or large intraorbital lesions often produce optic disc swelling?
4. Is there usually pain on eye movement with compressive optic neuropathy?
5. Is cupping uncommon in chronic compressive optic neuropathy?
6. What neuroimaging studies should be obtained for suspected compressive optic neuropathy?
7. Are episodes of transient monocular visual loss common in optic nerve sheath meningiomas?
 1
1
Neuro-ophthalmology Questions of the Week: Compressive and Infiltrative Optic Neuropathies
Questions:
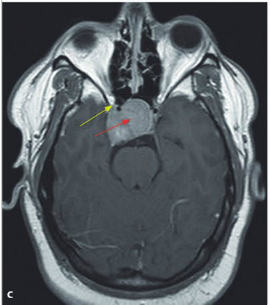
1. What is the most common cause of compressive optic neuropathy?
2. Are pilocytic astrocytoma and optic nerve glioma more common in adults or children?
3. Do anterior or large intraorbital lesions often produce optic disc swelling?
4. Is there usually pain on eye movement with compressive optic neuropathy?
5. Is cupping uncommon in chronic compressive optic neuropathy?
6. What neuroimaging studies should be obtained for suspected compressive optic neuropathy?
7. Are episodes of transient monocular visual loss common in optic nerve sheath meningiomas?
 1
1
Neuro-ophthalmology Question of the Week: Arteritic Anterior and Posterior Ischemic Optic Neuropathy
Question:
Which of the following are correct for giant cell arteritis?
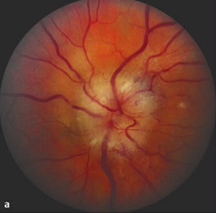
1. Visual loss may be preceded by recurrent episodes of transient monocular visual loss.
2. Visual loss may be preceded by recurrent episodes of transient diplopia.
3. AION is its most common ophthalmic manifestation.
4. It is the most common cause of PION.

Neuro-ophthalmology Questions of the Week: Posterior Ischemic Optic Neuropathy
Questions:
1. What is the typical visual field defect in nonarteritic PION?
2. Is disc swelling usually seen with nonarteritic PION?
3. What does PION not associated with surgery in patients older than age 50 generally indicate?
4. What should be ruled-out in non-operative PION in patients under 50?
 1
1
Neuro-ophthalmology Question of the Week-Optic Neuropathies
Question:
Which of the following statements are correct?
1. Anterior ischemic optic neuropathies are considered the equivalent of a “stroke of the optic nerve”.
2. The causes and mechanisms of anterior ischemic optic neuropathies and stroke are different.
3. The workup of a patient with an ischemic optic neuropathy is not the same as that for patients with retinal or cerebral infarction.
4. The clinician’s primary role in ischemic optic neuropathies is to exclude giant cell arteritis, control vascular risk factors, treat anemia, and prevent hypotension (e.g., in the setting of dialysis).
5. Anterior ischemic optic neuropathies are not associated with ipsilateral internal carotid artery stenosis and embolic AION is extremely rare.
6. Medications, such as amiodarone, may induce an optic neuropathy often indistinguishable from AION.
 1
1
Neuro-ophthalmology Questions of the Week: Optic Neuropathies
Questions:
1. What is the most common optic neuropathy in patients over age 50?
2. Why are altitudinal visual field defects common in ischemic optic neuropathies?
3. Do emboli commonly cause ischemic optic neuropathy?
 1
1
Neuro-ophthalmology Questions of the Week-Neuroretinitis
Questions:
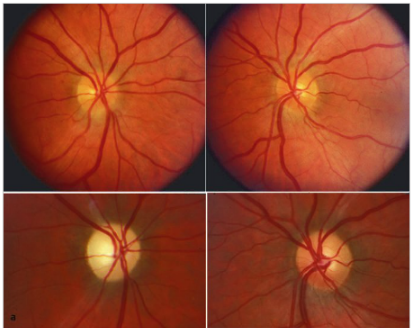
1. What are the ophthalmoscopic characteristics of neuroretinitis?
2. Is neuroretinitis caused by demyelination?
3. In what settings does neuroretinitis most commonly occur?
 1
1
Neuro-ophthalmology Question of the Week: Secondary Demyelinating Processes & Optic Neuritis
Questions:
1. When inflammatory optic neuritis is not associated with a primary demyelinating process in the optic nerve or the central nervous system what is the likely cause?
2. When inflammatory optic neuritis is not associated with a primary demyelinating process in the optic nerve or the central nervous system what should drive the work-up?
3. Is optic neuritis common in secondary and tertiary syphilis?
4. How is syphilitic optic neuritis treated and what is its prognosis?
5. What should be done all patients with HIV and optic neuritis?
 1
1
Neuro-ophthalmology Question of the Week-Acute Disseminated Encephalomyelitis (ADEM)
Questions:
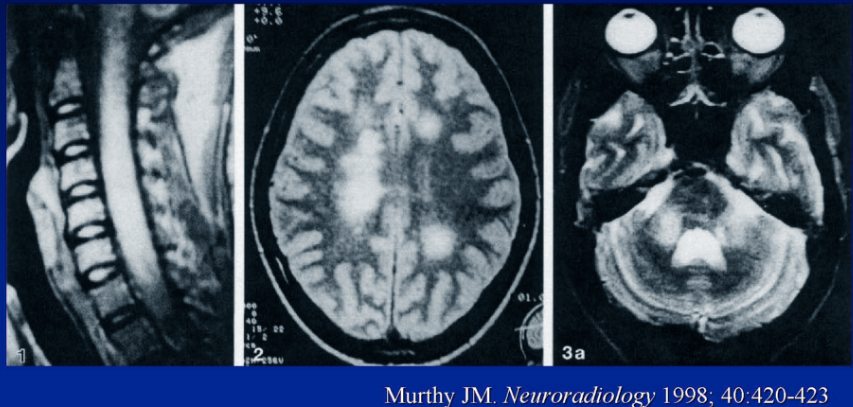
1. Is ADEM more common in in children or adults?
2. What may the clinical symptoms and MRI changes of ADEM mimic?
3. How many symptomatic episodes of ADEM is a patient likely to experience?
4. Is optic neuritis seen in some patients with ADEM?
 1
1