Questions:
1. When inflammatory optic neuritis is not associated with a primary demyelinating process in the optic nerve or the central nervous system what is the likely cause?
2. When inflammatory optic neuritis is not associated with a primary demyelinating process in the optic nerve or the central nervous system what should drive the work-up?
3. Is optic neuritis common in secondary and tertiary syphilis?
4. How is syphilitic optic neuritis treated and what is its prognosis?
5. What should be done all patients with HIV and optic neuritis?
 1
1
____________________________________________________
Questions with answers:
1. When inflammatory optic neuritis is not associated with a primary demyelinating process in the optic nerve or the central nervous system what is the likely cause?
A systemic infection or a systemic inflammatory disease.
2. When inflammatory optic neuritis is not associated with a primary demyelinating process in the optic nerve or the central nervous system what should drive the work-up?
The systemic symptoms and signs, patients’ characteristics, and associated ocular findings such as neuroretinitis should direct the subsequent workup.
3. Is optic neuritis common in secondary and tertiary syphilis?
Yes, optic neuritis common in secondary and tertiary syphilis.
4. How is syphilitic optic neuritis treated and what is its prognosis?
Syphilitic optic neuritis is treated like neurosyphilis. The visual prognosis is usually good.
5. What should be done all patients with HIV and optic neuritis?
A lumbar puncture should always be performed in patients with HIV and the CSF should be evaluated for likely causes of infections and malignancies (e.g., lymphoma) common in patients with HIV. Most opportunistic infections invading the CNS can produce an optic neuritis. Classic causes of such Infections are cytomegalovirus, toxoplasmosis, and cryptococcus.
Explanation:
“8.4.8 Other Causes of Optic Neuritis
Less commonly, inflammatory optic neuritis is not associated with a primary demyelinating process in the optic nerve or the central nervous system (CNS). Instead, the condition develops in the setting, or as the presenting manifestation, of a systemic infection or a systemic inflammatory disease.
Systemic symptoms and signs, patients’ characteristics, and associated ocular findings such as neuroretinitis should direct the subsequent workup.
Syphilitic Optic Neuritis
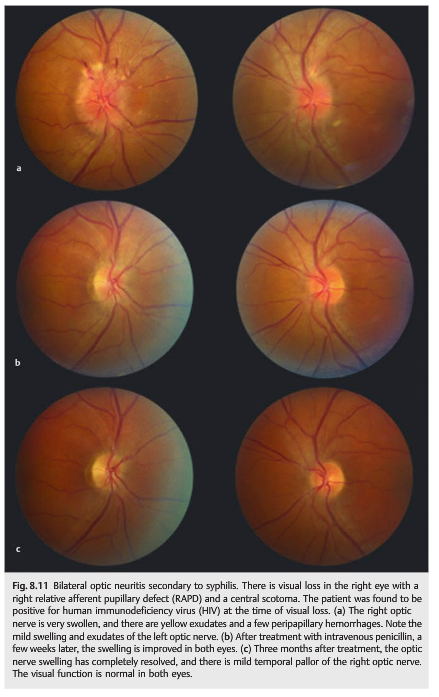
Optic neuritis is common in secondary and tertiary syphilis. It is usually associated with lymphocytic meningitis and is a sign of neurosyphilis. Raised intracranial pressure with papilledema is common with syphilitic lymphocytic meningitis. Testing for syphilis(rapid plasma reagin [RPR] and fluorescent treponemal antibody absorption [FTA-ABS]) should be considered in patients with optic neuritis. When blood tests are positive, a lumbar puncture (with opening pressure, CSF analysis, and Venereal Disease Research Laboratories [VDRL] testing) and HIV testing are mandatory. Syphilitic optic neuritis is treated like neurosyphilis. The visual prognosis is usually good (▶Fig. 8.11).
Optic Neuritis in Patients with HIV
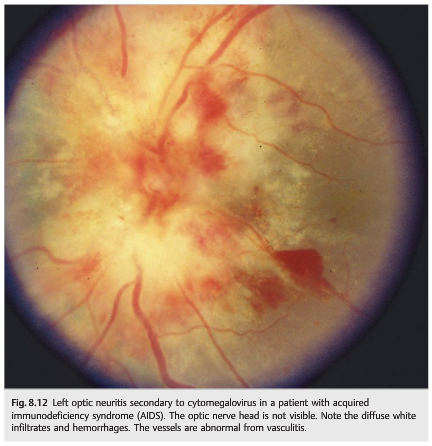
Optic neuritis is a not uncommon cause of visual loss in patients infected with HIV (see Chapter 20). Syphilis is the most common cause of optic neuritis in patients with HIV. Most opportunistic infections invading the CNS can produce an optic neuritis. Infections by cytomegalovirus, toxoplasmosis, and cryptococcus are the most classic causes. A lumbar puncture should always be performed, and CSF should be evaluated for all causes of infections and malignancies (e.g., lymphoma) common in patients with HIV(▶Fig. 8.12).
Sarcoid Optic Neuritis
Sarcoid optic neuritis may be isolated, or it may develop in a patient with neurosarcoidosis (see discussion in Chapter 20). The lumbar puncture often shows abnormal CSF (lymphocytic meningitis), and the MRI scan typically demonstrates intense gadolinium enhancement of the affected optic nerve. There is sometimes associated meningeal enhancement.Workup (general examination, ACE level, chest radiograph, chest computed tomography [CT], gallium scan, or fluorodeoxyglucose positron-emission tomography [FDG-PET] scan) may suggest systemic sarcoidosis. Biopsy of a lesion (usually skin lesion, lymph node, pulmonary lesion, or lacrimal gland) confirms the diagnosis of sarcoidosis.In sarcoidosis, the optic neuritis may result from lymphocytic meningitis present in neurosarcoidosis. Uni- or bilateral optic nerve edema may be present if there is raised intracranial pressure. Optic neuritis may also result from granulomatous infiltration of the optic nerve head associated with elevation of the optic nerve. Retinal lesions (infiltrates, vasculitis) and vitreous cells are common in this setting. Another cause is granulomatous infiltration of the intracranial portion of the optic nerve and the chiasm.
In most cases, the optic neuropathy responds well to corticosteroids and may be steroid-dependent, requiring long-term treatment with an immunosuppressive agent (▶Fig. 8.13).
 ”1
”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.