Question:
Which of the following statements are correct?
1. Anterior ischemic optic neuropathies are considered the equivalent of a “stroke of the optic nerve”.
2. The causes and mechanisms of anterior ischemic optic neuropathies and stroke are different.
3. The workup of a patient with an ischemic optic neuropathy is not the same as that for patients with retinal or cerebral infarction.
4. The clinician’s primary role in ischemic optic neuropathies is to exclude giant cell arteritis, control vascular risk factors, treat anemia, and prevent hypotension (e.g., in the setting of dialysis).
5. Anterior ischemic optic neuropathies are not associated with ipsilateral internal carotid artery stenosis and embolic AION is extremely rare.
6. Medications, such as amiodarone, may induce an optic neuropathy often indistinguishable from AION.
 1
1
____________________________________________________
Answer: each statement is correct.
Explanation: “Pearls
Although ischemic optic neuropathies are considered the equivalent of a “stroke of the optic nerve,” they cannot be directly compared with cerebral infarctions. The causes and mechanisms of ischemic optic neuropathies are different, and the workup of a patient with an ischemic optic neuropathy is not the same as that for patients with retinal or cerebral infarction.
8.5.2 Classification
Ischemic optic neuropathies include anterior ischemic optic neuropathy (AION), which is always associated with disc edema, and posterior ischemic optic neuropathy (PION), when the optic nerve appears normal acutely. AION is much more common than PION, accounting for 90% of cases of optic nerve ischemia. Ischemic optic neuropathies are categorized as nonarteritic ischemic optic neuropathy and arteritic ischemic optic neuropathy (usually in the setting of giant cell arteritis).Patients with giant cell arteritis and ischemic optic neuropathy are in danger of catastrophic, irreversible, bilateral total blindness that may be prevented by prompt treatment with corticosteroid therapy.
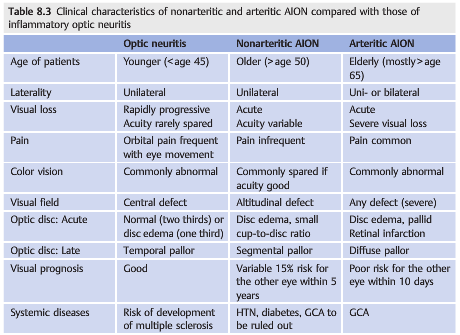
It is essential to correctly diagnose patients with ischemic optic neuropathies. Indeed, inflammatory optic neuritis is often over diagnosed in patients with acute optic neuropathy, especially in patients younger than 50. A brain MRI scan is usually obtained in these patients, who may be found to have one hyperintensity on the T2-weighted images. This inappropriately prompts a diagnosis of optic neuritis and presumed multiple sclerosis with dramatic consequences for the patient’s life and treatment. In addition, when ischemic optic neuropathy is missed, then giant cell arteritis may also be overlooked (▶Table 8.3).
8.5.3 Nonarteritic Anterior Ischemic Optic Neuropathy
Characteristics
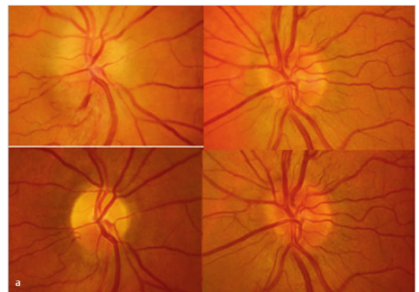
Nonarteritic AION (▶Fig. 8.19) is most common in Caucasians older than age 50.
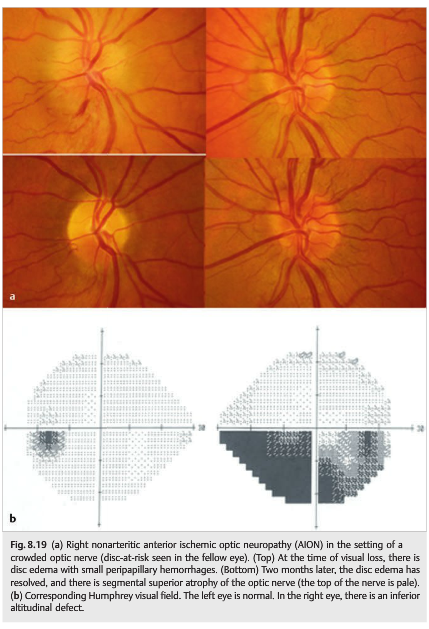
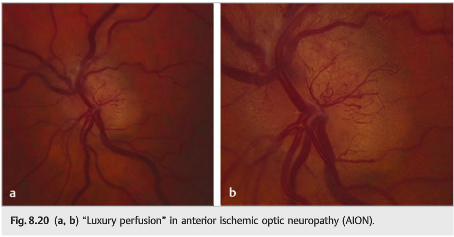
It is characterized by acute, painless monocular loss of vision that may progress over several hours or days. There is a RAPD and optic disc swelling, frequently with peripapillary hemorrhages. Gradually over weeks the optic disc develops pallor, and the edema resolves. Occasionally, disc swelling may be seen prior to visual loss (incipient AION). The typical visual field defect is altitudinal or arcuate, especially inferiorly. Acutely, some patients develop “luxury perfusion” of the ischemic optic nerve head, seen as dilated capillaries on the disc edema, or adjacent to the optic nerve pallor (▶Fig. 8.20).
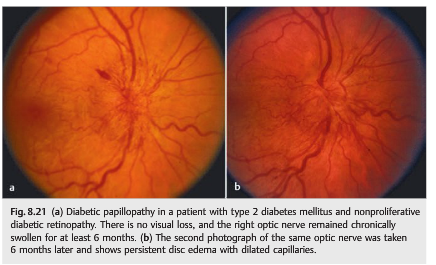
Diabetic papillopathy is believed to be an atypical form of AION that usually occurs in young patients with insulin-dependent diabetes. It is distinguished from typical nonarteritic AION by the slight degree (or even absence) of visual loss, the frequency of bilateral involvement (50%), the long duration of disc edema, and the good visual outcome (▶Fig. 8.21).
Causes
Although nonarteritic AION results from vascular occlusive disease of small vessels supplying the anterior portion of the optic nerve, its exact cause remains unclear. Anatomical factors such as a congenitally small and crowded optic nerve head with a small cup-to-disc ratio (so-called disc-at-risk) may mechanically contribute to the vascular event. As a disease of the small vessels, nonarteritic AION is not associated with ipsilateral internal carotid artery stenosis, and embolic AION is extremely rare.
Risk Factors
Proposed risk factors for nonarteritic AION include the following:
● Small, crowded disc (disc-at-risk)
● Other abnormalities localized to the disc
– Optic nerve head drusen
– Anomalous disc
–Severe papilledema
● Severe hypotension
– Operative
– Systemic massive hemorrhage
– Cardiac arrest
– Renal dialysis
● Severe anemia
● Hypercoagulable disorders
● Radiation optic neuropathy
● Acute intraocular hypertension (during ocular surgery, after an intravitreal injection of steroids, or during an attack of angle-closure glaucoma)
● Vascular risk factors for atherosclerosis are commonly found in AION patients.
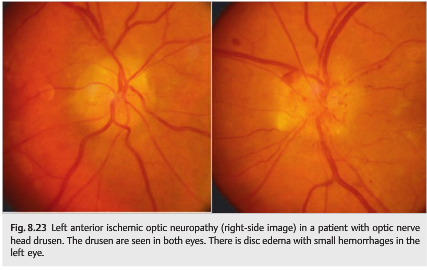
In rare cases, AION may occur in a patient with optic nerve head drusen or papilledema. The drusen or the papilledema makes the optic nerve head more crowded and may “choke” the optic nerve head, which becomes ischemic (▶Fig. 8.23). Medications, such as amiodarone, may induce an optic neuropathy often indistinguishable from AION.
Pearls
Nonarteritic AION is not an embolic disorder. Evaluation of the internal carotid artery is not indicated in isolated, typical AION. There is no definite increased risk of cerebrovascular disease in the population of patients with AION, but vascular risk factors are common and should be controlled.
Natural History
Up to 50% of patients retain visual acuity of 20/60 or better. Recurrences in the same eye are rare (<5%). Subsequent involvement of the fellow eye is about 15% at 5 years in patients with a disc-at-risk.
Treatment
There is no established treatment for nonarteritic AION. The clinician’s primary role is to exclude giant cell arteritis, control vascular risk factors, treat anemia, and prevent hypotension (e.g., in the setting of dialysis).”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.