Questions:
1. What is the most common cause of compressive optic neuropathy?
2. Are pilocytic astrocytoma and optic nerve glioma more common in adults or children?
3. Do anterior or large intraorbital lesions often produce optic disc swelling?
4. Is there usually pain on eye movement with compressive optic neuropathy?
5. Is cupping uncommon in chronic compressive optic neuropathy?
6. What neuroimaging studies should be obtained for suspected compressive optic neuropathy?
7. Are episodes of transient monocular visual loss common in optic nerve sheath meningiomas?
 1
1
____________________________________________________
Questions with answers:
1. What is the most common cause of compressive optic neuropathy?
Pituitary tumors are the most common cause of compressive optic neuropathy.
2. Are pilocytic astrocytoma and optic nerve glioma more common in adults or children?
Pilocytic astrocytoma and optic nerve glioma are more common and more benign in children than in adults.
3. Do anterior or large intraorbital lesions often produce optic disc swelling?
Anterior or large intraorbital lesions often produce optic disc swelling whereas intracranial, intracanalicular, and posterior orbital compressive lesions typically do not produce disc swelling.
4. Is there usually pain on eye movement with compressive optic neuropathy?
Usually, there no pain with eye movements.
5. Is cupping uncommon in chronic compressive optic neuropathy?
Cupping of the optic nerves is not uncommon in chronic compression.
6. What neuroimaging studies should be obtained for suspected compressive optic neuropathy?
Dedicated views of the orbits, the sella turcica, or the cavernous sinus are necessary and should be obtained based on clinical suspicion. MRI with contrast is preferred.
7. Are episodes of transient monocular visual loss common in optic nerve sheath meningiomas?
Optic nerve sheath meningiomas arise from the dural sheath of the optic nerve. This tumor occurs mostly in middle-aged women who present with unilateral, painless, progressive loss of vision in one eye. Episodes of transient monocular visual loss are common.
Explanation: “8.6 Compressive and Infiltrative Optic Neuropathies
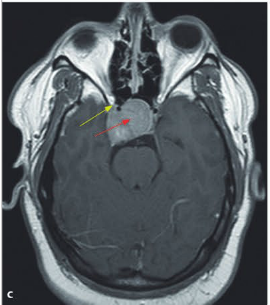
Various lesions may compress or infiltrate the intraorbital, intracranial, or prechiasmal optic nerves. Anterior or large intraorbital lesions often produce optic disc swelling (▶Fig. 8.26), whereas intracranial, intracanalicular, and posterior orbital compressive lesions typically do not produce disc swelling.
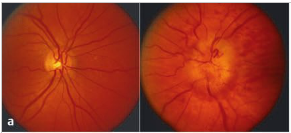
Fig.8.26 (a) Left optic nerve sheath meningioma (on the right) with optic disc edema.

Fig.8.26 (b) Left central scotoma on Goldmann visual fields (on the left).
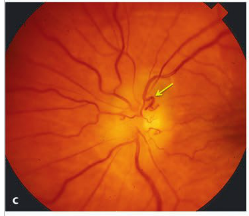
Fig.8.26 (c) A few months later, the left optic nerve is pale with residual mild disc edema and more obvious optociliary shunt vessels (arrow).
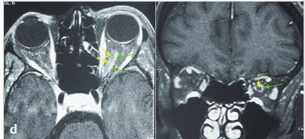
Fig.8.26 (d) T1-weighted axial (left)and coronal (right) magnetic resonance imaging of the orbits with fat suppression and with contrast showing the left optic nerve sheath meningioma. There is enhancement of the optic nerve sheath (green arrow), whereas the optic nerve itself (yellow arrow) does not enhance.
8.6.1 Characteristics
The clinical presentation varies based on the type and location of the mass:
● Progressive unilateral optic neuropathy (progressive visual loss with abnormal color vision, visual field defect, and optic disc pallor or disc edema)
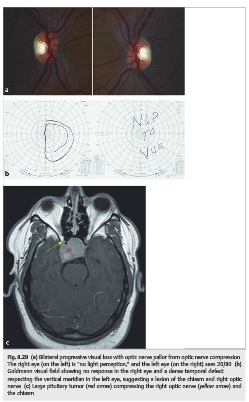
● Intracranial lesions in the region of the chiasm that may produce vision loss in both eyes (bilateral optic neuropathies, bitemporal hemianopia, junctional scotoma)
● Usually, no pain with eye movements
● Headache if raised intracranial pressure (large tumor, hydrocephalus) or involvement of branches of the trigeminal nerve (cavernous sinus)
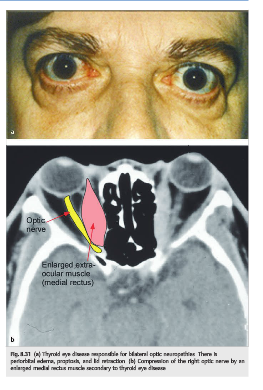
● Proptosis and diplopia common in orbital lesions
● Cranial nerve palsies common in lesions extending into the cavernous sinus
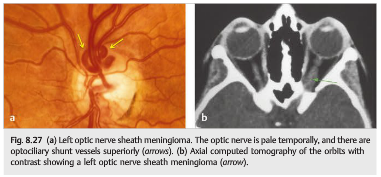
Optociliary shunt vessels may develop as a result of optic nerve compression(▶Fig. 8.27).
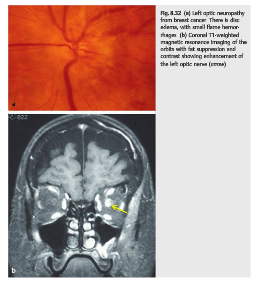
The optic nerve may also be compressed or infiltrated by neoplasm (▶Fig. 8.28,▶Fig. 8.29, ▶Fig. 8.30, ▶Fig. 8.31, ▶Fig. 8.32, ▶Fig. 8.33, ▶Fig. 8.34, ▶Fig. 8.35) or by an inflammatory process, such as orbital inflammatory pseudotumor or thyroid eye disease (see▶Fig. 8.31).(▶Fig. 8.35) or by an inflammatory process, such as orbital inflammatory pseudotumor or thyroid eye disease.

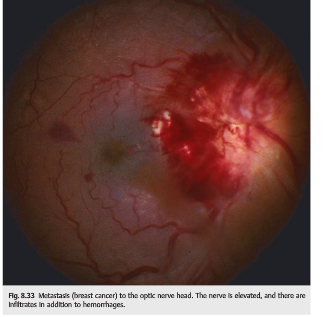
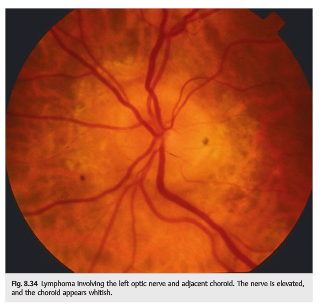
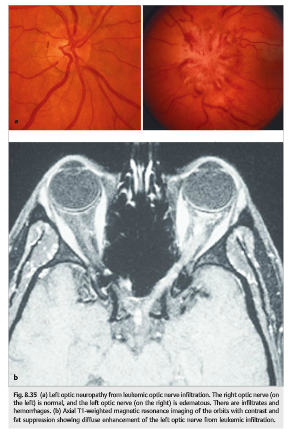
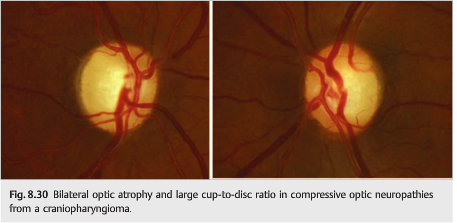
Cupping of the optic nerves is not uncommon in chronic compression. There is pallor of the remaining rim, unlike in glaucomatous nerve cupping, in which the cups are large with retained pink rims (▶Fig. 8.30).
8.6.2 Causes
Causes of compressive optic neuropathy include the following:
● Neoplastic
○ Optic nerve sheath meningioma
○ Intraorbital tumor (hemangioma, lymphangioma, metastasis, etc.)
○ Sphenoid meningioma
○ Pituitary tumor○ Craniopharyngioma
● Non-neoplastic
○ Thyroid eye disease
○ Orbital pseudotumor
○ Orbital hemorrhage
○ Paget disease
○ Fibrous dysplasia
○ Ophthalmic artery aneurysm
○ Ectatic internal carotid artery
● Neoplastic
○ Optic nerve glioma
○ Metastatic carcinoma
○ Nasopharyngeal carcinoma and other contiguous tumors
○ Lymphoma○ Leukemia
○ Meningeal carcinomatosis
● Non-neoplastic
○ Sarcoidosis
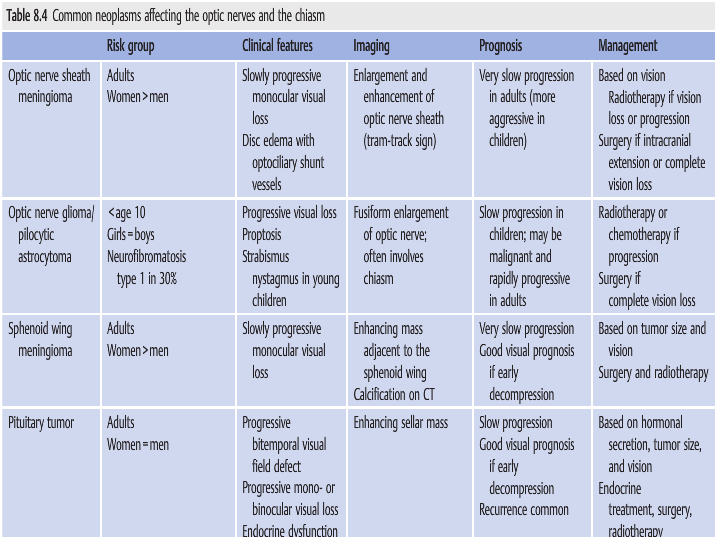
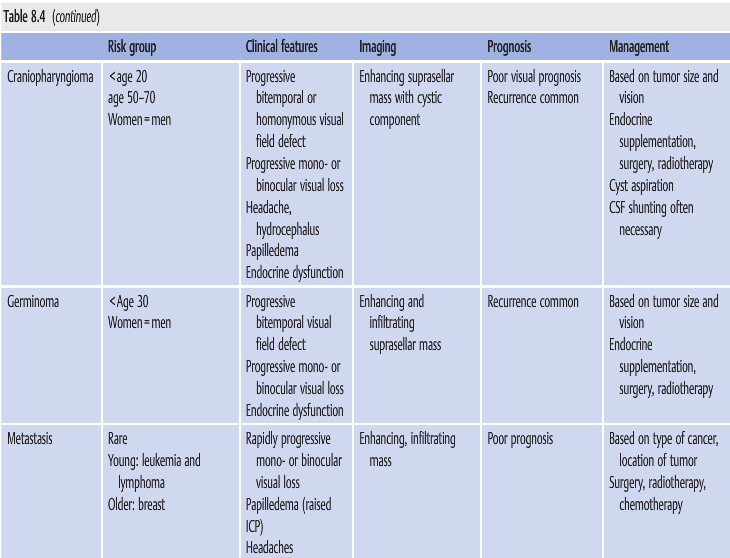
Causes of infiltrative optic neuropathy (▶Table 8.4)
Pearls
The diagnosis of compressive optic neuropathy is confirmed by imaging. However, tumors compressing the anterior visual pathways may be missed on routine brain CT or MRI. Dedicated views of the orbits, the sella turcica, or the cavernous sinus are necessary and should be obtained based on clinical suspicion. MRI with contrast is preferred.
8.6.3 Diagnosis
In most cases, a presumed diagnosis of compressive or infiltrative optic neuropathy is made based on clinical presentation and neuroimaging. A biopsy is the only way to obtain a definite diagnosis, but it is rarely possible in optic nerve tumors or optic nerve sheath meningiomas because optic nerve biopsy usually results in permanent visual loss. In many of these cases, treatment is based on the presumed diagnosis.
Optic nerve sheath meningiomas arise from the dural sheath of the intraorbital optic nerve. This tumor occurs mostly in middle-aged women who present with unilateral,painless, progressive loss of vision in one eye. Episodes of transient monocular visual loss are common. The optic disc is often already pale at the time of diagnosis, and it may be swollen. There may be optociliary shunt vessels on the optic disc (dilated veins resulting from chronic central retinal vein compression) (Fig. 8.27).
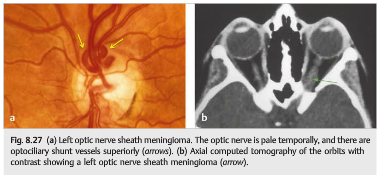
Imaging often misses optic nerve sheath meningiomas, which can be difficult to visualize, especially if there are no dedicated orbital images with fat suppression and contrast. Without treatment, the vision deteriorates, and the tumor may even extend intracranially through the optic canal. However, its progression is very slow, and treatment is based on the amount of visual loss and the size of the tumor.Prognosis is mostly based on the type and location of the tumor, as well as the duration of visual loss. Vision often improves (at least partially) after treatment.
Pilocytic astrocytoma and optic nerve glioma are more common and more benign in children than in adults.
Pituitary tumors are the most common cause of compressive optic neuropathy.
Pearls
Low-tension glaucoma is a rare type of glaucoma in which patients with normal intraocular pressure develop a glaucomatous optic neuropathy. It is a diagnosis of exclusion, and other causes of optic neuropathies, particularly compressive, need to be ruled out by neuroimaging.”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.