Questions:
1. Are cases of toxic or nutritional optic neuropathies likely to be caused by a single agent?
2. Is vision likely to recover with discontinuation of the toxin or vitamin deficiency supplementation?
3. What are the common agents that cause toxic optic neuropathies?
4. What are the common agents that cause nutritional optic neuropathies?
5. What condition do the fundus findings of amiodarone toxicity often resemble?
6. What should always be checked in patients with progressive bilateral visual loss and bilateral optic atrophy?
 1
1
____________________________________________________
Correct Answers:
1. Are cases of toxic or nutritional optic neuropathies likely to be caused by a single agent? Definitively proven cases of optic nerve damage caused by a single recognized toxic agent or a deficiency in a single identified nutrient are rare.
2. Is vision likely to recover with discontinuation of the toxin or vitamin deficiency supplementation?
In some cases, discontinuation of the agent or vitamin supplementation results in improvement of visual function. However, visual loss is often irreversible.
3. What are the common agents that cause toxic optic neuropathies?
Suspected toxins linked to optic neuropathies are methanol, ethylene glycol, cobalt, lead, zinc, organic solvents, toluene, tobacco (usually, cigars), ethambutol, amiodarone, linezolid, and disulfiram.
4. What are the common agents that cause nutritional optic neuropathies?
Nutritional causes include vitamin B12, folate, and copper deficiencies.
5. What condition do the fundus findings of amiodarone toxicity often resemble?
Amiodarone toxicity is classically associated with disc edema resembling nonarteritic anterior ischemic optic neuropathy. Visual loss may be subacute or slowly progressive. Visual function may improve after discontinuation of the medication (which should be done only after consulting with the patient’s cardiologist).
6. What should always be checked in patients with progressive bilateral visual loss and bilateral optic atrophy?
Always check vitamin B12 and copper levels in patients with progressive bilateral visual loss and bilateral optic atrophy.
Explanation: “8.8 Toxic and Nutritional Optic Neuropathies
Toxic and nutritional optic neuropathies generally have similar clinical features and may even coexist in the same patient.
8.8.1 Features
Characteristic clinical features include progressive, symmetrical central visual loss; reduced perception of color; and cecocentral scotomas. Acutely, the optic nerve may be normal or may appear slightly swollen. Temporal optic disc pallor is seen at least 6weeks after the onset of visual loss.
8.8.2 Causes
Causation in many cases is likely multifactorial. In humans, definitively proven cases of optic nerve damage caused by a single recognized toxic agent or a deficiency in a single identified nutrient are rare. In some cases, discontinuation of the agent or vitamin supplementation may result in improvement of visual function. However, visual loss is often irreversible.
Among the suspected toxins linked to optic neuropathies are methanol, ethylene glycol, cobalt, lead, zinc, organic solvents, toluene, tobacco (usually, cigars), ethambutol, amiodarone, linezolid, and disulfiram. Nutritional causes include vitamin B12, folate, and copper deficiencies. Several of the leading types of toxic and nutritional optic neuropathies are described in the following section.
8.8.3 Types
Methanol
Methanol ingestion is the most widely recognized cause of toxic optic neuropathy. It is also most often accidental (mistaken for or added to ethyl alcohol). Methanol-related optic neuropathy is acute, and the optic nerves are usually swollen. Visual loss from bilateral optic neuropathies is associated with headaches and nausea. Worse visual loss, abdominal pain, respiratory distress, confusion, and, ultimately, coma, and death happen 18 to 48 hours after ingestion. Metabolic acidosis is one of the hallmarks of methanol ingestion.
Ethylene Glycol
Ethylene glycol is the active ingredient in automobile antifreeze. It may be consumed accidentally or in a suicide attempt. It is very toxic to the optic nerves. Symptoms and signs resemble those of methanol intoxication, except for renal insufficiency, which is common with ethylene glycol.
Ethambutol
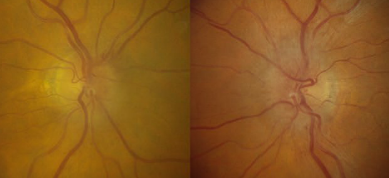
Ethambutol, an antimycobacterial drug used to treat tuberculosis, is the medication most often implicated in toxic optic neuropathy (▶Fig. 8.38).
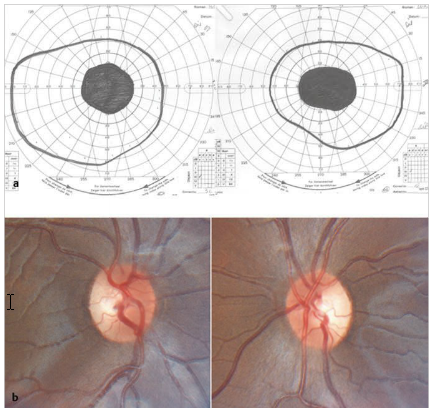
Fig.8.38 (a) Goldmann visual field showing bilateral cecocentral scotoma in a patient treated with ethambutol for tuberculosis. (b) Bilateral temporal pallor of the optic nerves from ethambutol toxicity.
Toxicity is usually dose related (develops in patients taking the drugs for a few months—usually at least 2months, with a mean of 7 months).Bitemporal visual field defects may reflect early involvement of the chiasm, and color vision is affected early. Visual loss is bilateral and slowly progressive. Visual function may improve after discontinuation of the drug.
Amiodarone
Although it is still debated, there is good evidence that sequential bilateral optic neuropathies may develop in patients treated with amiodarone, an antiarrhythmic agent. Toxicity is dose related and usually occurs in patients who have been treated with it for a few months. It is classically associated with disc edema resembling nonarteritic anterior ischemic optic neuropathy (▶Fig. 8.39). Visual loss may be subacute or slowly progressive. Visual function may improve after discontinuation of the medication (which can be done only after consulting with the patient’s cardiologist.
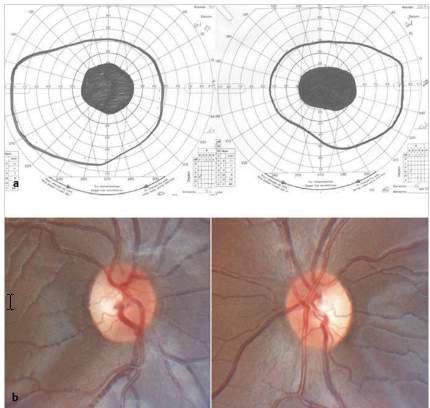
Fig.8.38 (a) Goldmann visual field showing bilateral cecocentral scotoma in a patient treated with ethambutol for tuberculosis. (b) Bilateral temporal pallor of the optic nerves from ethambutol toxicity.
Toxicity is usually dose related (develops in patients taking the drugs for a few months—usually at least 2months, with a mean of 7 months).Bitemporal visual field defects may reflect early involvement of the chiasm, and color vision is affected early. Visual loss is bilateral and slowly progressive. Visual function may improve after discontinuation of the drug.
Amiodarone
Although it is still debated, there is good evidence that sequential bilateral optic neuropathies may develop in patients treated with amiodarone, an antiarrhythmic agent. Toxicity is dose related and usually occurs in patients who have been treated with it for a few months. It is classically associated with disc edema resembling nonarteritic anterior ischemic optic neuropathy (▶Fig. 8.39). Visual loss may be subacute or slowly progressive. Visual function may improve after discontinuation of the medication (which can be done only after consulting with the patient’s cardiologist.
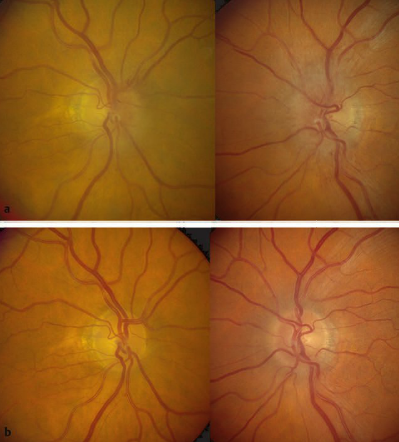
Fig.8.39 (a) Bilateral disc edema (worse in the left eye) in a patient treated with amiodarone for atrial fibrillation who developed visual loss in his left eye. (b) One month after discontinuing the amiodarone, the disc edema has resolved and his visual function has improved.
Pearls
The diagnosis of toxic optic neuropathy is usually a diagnosis of exclusion. Workup ruling out other causes of bilateral optic neuropathies, such as compression, vitamin B12 Deficiency, and hereditary optic neuropathies, should always be obtained.
Vitamin B12 Deficiency
Severe vitamin B12 deficiency (usually from impaired absorption) may produce bilateral, slowly progressive optic neuropathies (▶Fig. 8.40). The optic neuropathies are often the first sign of vitamin B12 deficiency and may precede the anemia and other neurologic symptoms and signs.
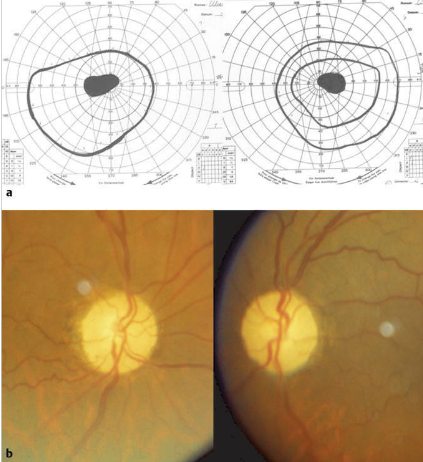
Fig.8.40 (a) Goldmann visual fields showing bilateral cecocentral scotomas from vitamin B12 Deficiency. (b) Bilateral optic atrophy.
Copper Deficiency
Chronic copper deficiency is very rare and can cause many hematological manifestations, such as myelodysplasia, anemia, leukopenia, and neutropenia, as well as ataxia,peripheral neuropathy, and bilateral optic neuropathies.
Pearls
Always check vitamin B12 and copper levels in patients with progressive bilateral visual loss and bilateral optic atrophy.”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.