Questions:
1. What is the typical visual field defect in nonarteritic PION?
2. Is disc swelling usually seen with nonarteritic PION?
3. What does PION not associated with surgery in patients older than age 50 generally indicate?
4. What should be ruled-out in non-operative PION in patients under 50?
 1
1
____________________________________________________
Questions with answers:
1. What is the typical visual field defect in nonarteritic PION?
The typical visual field defect is altitudinal or arcuate, especially inferiorly.
2. Is disc swelling usually seen with nonarteritic PION?
Disc swelling is not seen with nonarteritic PION.
3. What does PION not associated with surgery in patients older than age 50 generally indicate?
Non-operative PION in patients older than age 50 is usually indicative of giant cell arteritis.
4. What should be ruled-out in non-operative PION in patients under 50?
In non-operative PION in patients under 50, compression of the posterior optic nerve is ruled out by a good-quality MRI scan of the orbits with contrast, along with an extensive systemic workup looking for an underlying systemic inflammatory disorder.
Explanation:
“8.5.4 Nonarteritic Posterior Ischemic Optic Neuropathy
Characteristics
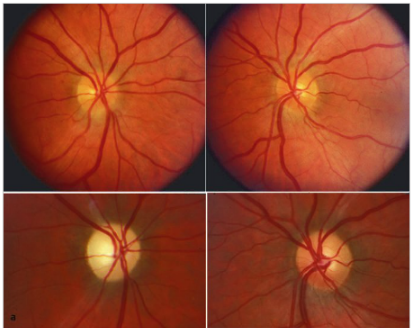
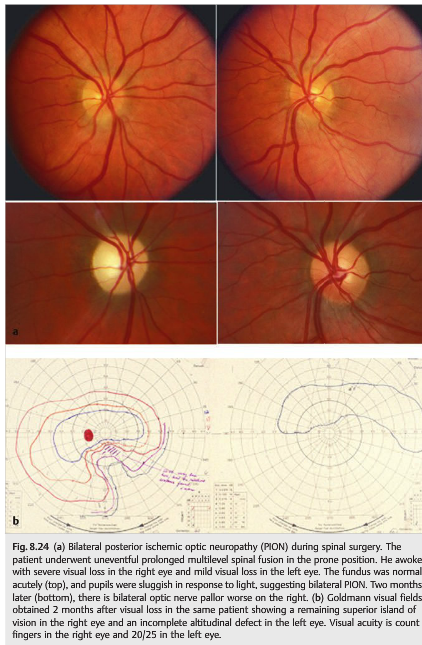
Nonarteritic PION (▶Fig. 8.24) is characterized by acute, painless monocular loss of vision that may progress over several hours or days. There is a RAPD. The optic disc is normal, initially. Gradually, over 4 to 6 weeks, the optic disc develops pallor. The typical visual field defect is altitudinal or arcuate, especially inferiorly.
“8.5.4 Nonarteritic Posterior Ischemic Optic Neuropathy
Characteristics
Nonarteritic PION (▶Fig. 8.24) is characterized by acute, painless monocular loss of vision that may progress over several hours or days. There is a RAPD. The optic disc is normal, initially. Gradually, over 4 to 6 weeks, the optic disc develops pallor. The typical visual field defect is altitudinal or arcuate, especially inferiorly.
Diagnosis and Causes
Nonarteritic PION is extremely rare and may occur during lengthy spinal and cardiac surgery or in patients with acute systemic hypotension. It is usually a diagnosis of exclusion made only after compression of the posterior optic nerve is ruled out by a good-quality MRI scan of the orbits with contrast, along with an extensive systemic workup looking for an underlying systemic inflammatory disorder. Non-operative PION in patients older than age 50 is usually indicative of giant cell arteritis.
Risk Factors
Presumed risk factors for nonarteritic PION include the following:
● Operative
o Spine (prone; long duration)
o Coronary artery bypass
● Severe hypotension
o Systemic hemorrhage
o Cardiac arrest
o Renal dialysis
● Severe anemia
● Hypercoagulable disorders
● Radiation optic neuropathy”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.