Questions:
1. What specific steps should be followed in examining a patient with anisocoria?
2. What are the characteristics of physiologic anisocoria?
3. What are the ocular causes of anisocoria?
____________________________________________________
Questions with answers:
1. What specific steps should be followed in examining a patient with anisocoria?
To determine the cause of anisocoria, the first step is to determine which pupil is abnormal—the large pupil or the small pupil—by carefully evaluating the pupillary reactions in the dark and in the light.
The next step is to look for associated symptoms and signs:
● A decreased palpebral fissure on the side of a small pupil suggests a Horner Syndrome.
● Diplopia, ptosis, and impaired extraocular movements on the side of a large pupil point to a third nerve palsy.
● An isolated large pupil without ptosis or diplopia suggests Adie pupil or pharmacologic mydriasis.
● With mydriasis, patients often complain of decreased near vision (from impaired accommodation) and of sensitivity to light.
2. What are the characteristics of physiologic anisocoria?
Physiologic anisocoria, a normal benign inequality of the pupils that may change from time to time, is seen in about 20% of the normal population.
● Reviewing the patient’s old photographs on a driver’s license or ID (with magnifying glasses or the slit lamp) may help confirm the diagnosis, as physiologic anisocoria is usually persistent.
● The amount of anisocoria is usually equal in light and dark (may be slightly greater in the dark than in the light).
● The anisocoria is usually <0.5mm.
● Depending on the degree of ambient lighting, the anisocoria may seem to come and go.
● Occasionally, the anisocoria may switch sides.
3. What are the ocular causes of anisocoria?
Ocular causes of anisocoria include: structural iris defects, congenital defects (aniridia, iris coloboma, ectopic pupils, persistent pupillary membrane, polycoria, heterochromia), and iridocorneal endothelial (ICE) syndrome
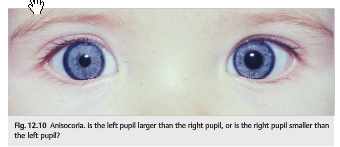
Explanation: “12.4 Anisocoria
Patients with anisocoria, or inequality in the size of the pupils, usually present emergently and generate much anxiety in the emergency room. Indeed, anisocoria from a third nerve palsy may reveal an intracranial aneurysm, which may rupture and cause life-threatening subarachnoid hemorrhage if not diagnosed promptly. The fear of an underlying life-threatening condition such as an intracranial aneurysm often leads physicians to obtain numerous tests. However, a simple and logical clinical approach that appreciates the mechanisms of anisocoria allows for prompt recognition of true emergencies and often avoids the need for invasive and costly testing in other cases.
12.4.1 Diagnosis
To determine the cause of anisocoria, the first step is to determine which pupil is abnormal—the large pupil or the small pupil—by carefully evaluating the pupillary reactions in the dark and in the light.
The next step is to look for associated symptoms and signs:
● A decreased palpebral fissure on the side of a small pupil suggests a Horner Syndrome.
● Diplopia, ptosis, and impaired extraocular movements on the side of a large pupil point to a third nerve palsy.
● An isolated large pupil without ptosis or diplopia suggests Adie pupil or pharmacologic mydriasis.
● With mydriasis, patients often complain of decreased near vision (from impaired accommodation) and of sensitivity to light (photophobia).
12.4.2 Causes of Anisocoria
Physiologic Anisocoria
Physiologic anisocoria, a normal benign inequality of the pupils that may change from time to time, is seen in about 20% of the normal population (▶Fig. 12.13).
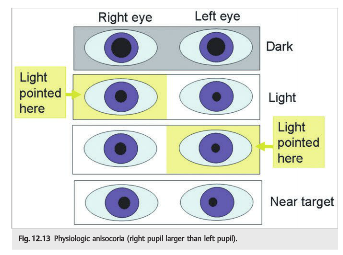
● Reviewing the patient’s old photographs on a driver’s license or ID (with magnifying glasses or the slit lamp) may help confirm the diagnosis, as physiologic anisocoria is usually persistent.
● The amount of anisocoria is usually equal in light and dark (may be slightly greater in the dark than in the light).
● The anisocoria is usually <0.5mm.
● Depending on the degree of ambient lighting, the anisocoria may seem to come and go.
● Occasionally, the anisocoria may switch sides.
Ocular Causes of Anisocoria
The ocular examination of the anterior segment by an ophthalmologist using a slit lamp confirms the diagnosis.
Structural defects of the iris can lead to anisocoria and abnormal pupillary shapes.
Congenital defects, such as aniridia, iris coloboma, congenital ectopic pupils, persistent pupillary membrane, polycoria, congenital heterochromia, iridocorneal endothelial (ICE) syndrome, and other developmental anomalies of the anterior segment, producer anisocoria, which usually presents in childhood.
Numerous acquired ocular conditions, such as intraocular inflammation (anterior uveitis), anterior segment ischemia, neovascularization of the iris, trauma, iris sphincter atrophy related to surgical or traumatic injury, mechanical distortion by an intraocular tumor, and angle closure glaucoma, also produce anisocoria. Associated visual loss, ocular redness, and ocular pain are usually present.
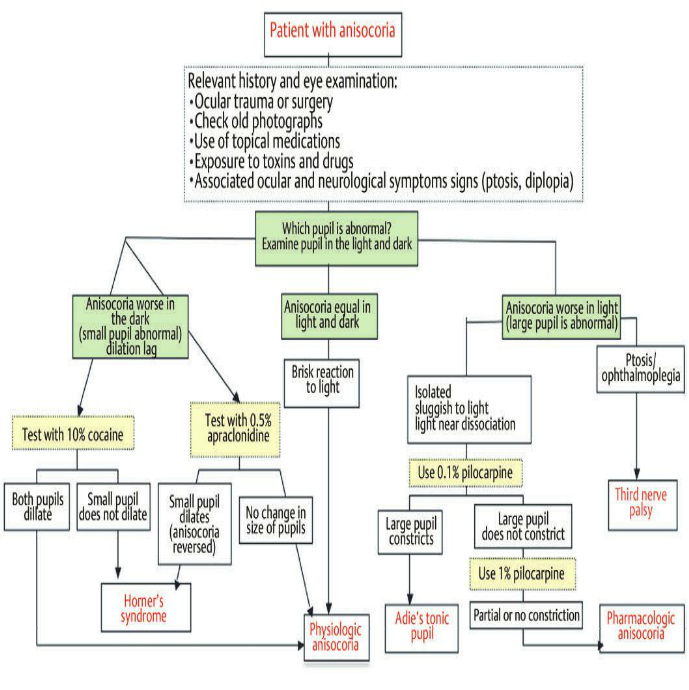
Fig.12.43 Approach to anisocoria”1
________________________________________________________
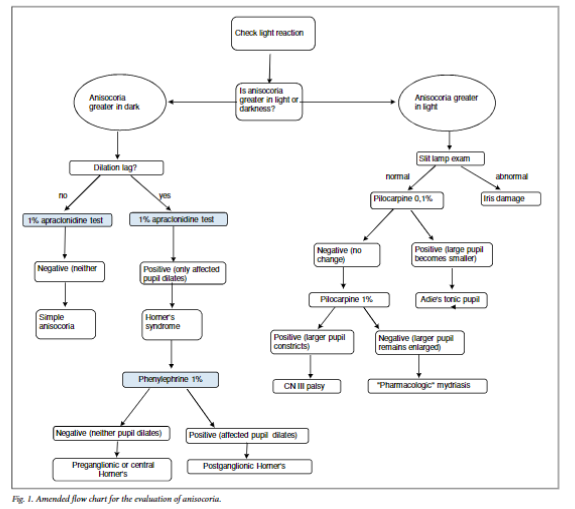
Alternate flow chart for the evaluation of anisocoria.2
References:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
2. Pharmacological testing in Horner’s syndrome – a new paradigm. Smit DP. S Afr Med J 2010; 100: 738-740.
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections totcooper@stanford.edu.