Questions:
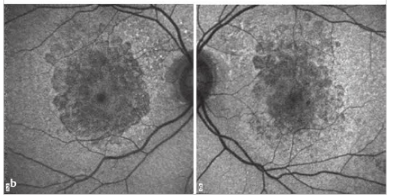
1. What are the symptoms of IIH?
2. What are the criteria for the diagnosis of IIH?
3. What is the ideal test when evaluating a patient with presumed papilledema?
4. A patient with papilledema has a normal brain MRI, what test should be done next?
5. What should one consider if the headaches of IIH do not improve (at least transiently) after lumbar puncture?
6. What does a normal Brain MRI in the setting of papilledema suggest?
7. What should be evaluated next in a patient with bilateral swollen discs, normal BP, normal CT with and without contrast, LP opening pressure >250mm and normal or abnormal CSF contents?
8. What should be evaluated next in a patient with bilateral swollen discs, normal BP, normal MRI with and without contrast, LP opening pressure >250mm and normal or abnormal CSF contents?
9. What are the main factors associated with IIH?
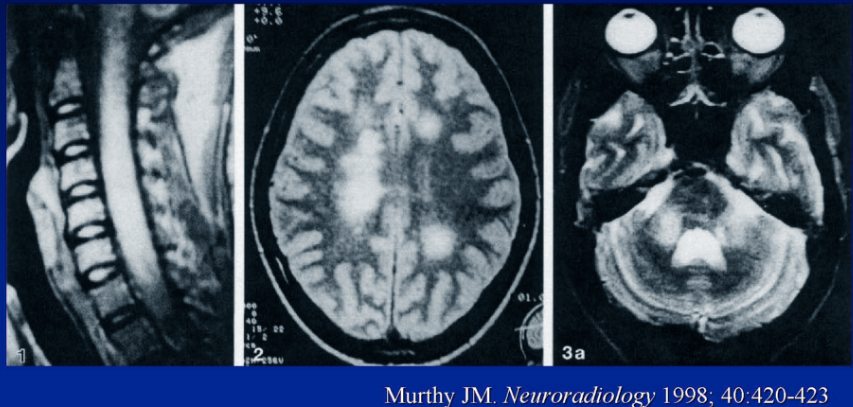
10. What condition can cerebral venous thrombosis mimic?
11. What can early recognition of cerebral venous thrombosis prevent?
12. Should papilledema from a meningeal process or cerebral venous thrombosis be classified as IIH?
13. What are the goals of the management of IIH?
14. What is basis for management of IIH?
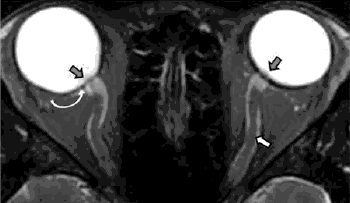
15. What MRI findings are supportive of the diagnosis of IIH?
 1
1 2
2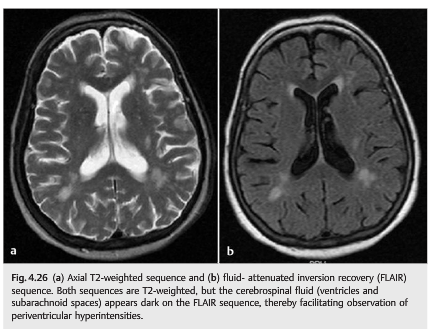
 1
1
 1
1 1
1 1
1 1
1