Question: Which of the following are correct?
1. Fat is hyperintense on T1.
2. Vitreous is hyperintense on T1.
3. CSF is hyperintense on T1.
4. Subacute blood is hyperintense on T1.
5. Fat is hypointense on T2.
6. Vitreous is hypointense on T2.
7. CSF is hypointense on T2.
8. Diffusion-weighted images are ideal in detecting acute cerebral ischemia.
9. T2 gradient echo allows better visualization of blood products, such as hemosiderin.
____________________________________________________
Answers:
1. Fat is hyperintense on T1.
4. Subacute blood is hyperintense on T1.
5. Fat is hypointense on T2.
8. Diffusion-weighted images are ideal in detecting acute cerebral ischemia.
9. T2 gradient echo allows better visualization of blood products, such as hemosiderin.
Explanation1: “Magnetic Resonance Imaging
MRI offers many advantages over CT and is the most commonly obtained ancillary test in neuro-ophthalmology. It provides excellent contrast resolution between soft tissues, and multiplanar imaging can be done without repositioning the patient.
Various sequences are obtained that allow visualization of different tissues. The appearance of the tissues varies based on the sequence used.
T1-weighted images provide good anatomical details. Fat looks bright (hyperintense), vitreous looks black (hypointense), cerebrospinal fluid (CSF) looks black (hypointense), and subacute blood appears white (hyperintense). On T1-weighted images, brain gray matter is gray, and brain white matter is lighter. Most cerebral parenchymal lesions appear dark (hypointense), unless gadolinium contrast is given; in that case, and if there is a breakdown in the blood–brain barrier, they may appear white (hyperintense).
The T1-weighted midline sagittal view is the first sequence systematically obtained on MRI, and it is very helpful in neuro-ophthalmology (▶Fig. 4.23).
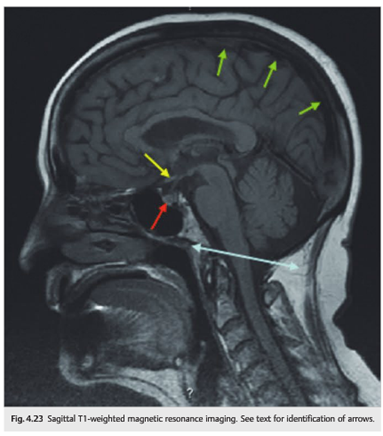
It provides information on the absence of cerebellar tonsillar herniation (Chiari malformation) (blue line in ▶Fig. 4.23), the pituitary gland (red arrow), the chiasm (yellow arrow), and the superior sagittal venous sinus (green arrows).
Because the orbits are filled with fat, a regular T1 sequence does not allow good evaluation of the orbits. In addition, administration of contrast results in enhancement of normal extraocular muscles and abnormal intraorbital structures; these appear brighter and therefore cannot be distinguished from the white orbital fat on a regular T1 sequence. A T1 sequence with fat suppression transforms the bright signal of the fat into a black signal and allows for very good orbital studies, before and after contrast administration (▶Fig. 4.24).
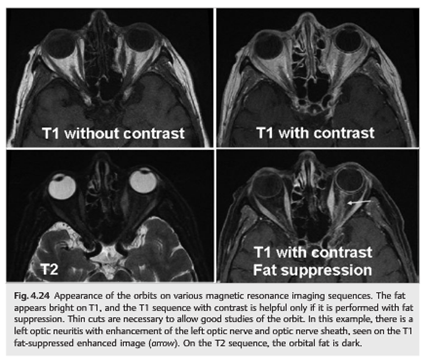
The orbits are best studied with a combination of axial and coronal views. Thin cuts are necessary.
Orbital MRI should include the following:
●Axial T1 sequence
●Axial T1 sequence with fat suppression
●Axial T1 sequence with fat suppression after injection of contrast
●Coronal T1 sequence with fat suppression
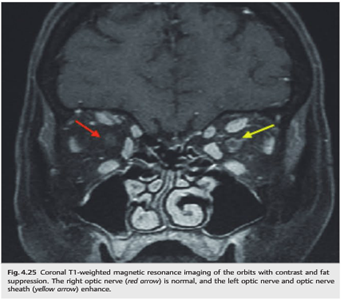
●Coronal T1 sequence with fat suppression after injection of contrast (▶Fig. 4.25)
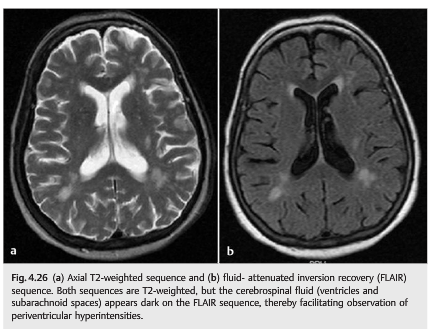
T2-weighted images are ideal for screening for brain parenchymal abnormalities. On T2-weighted images, fat looks darker (hypointense), vitreous looks bright (hyperintense), ventricles (CSF) look bright (hyperintense), and brain gray matter is lighter than brain white matter. Additionally, most cerebral parenchymal lesions appear bright (hyperintense), especially inflammatory or ischemic lesions.
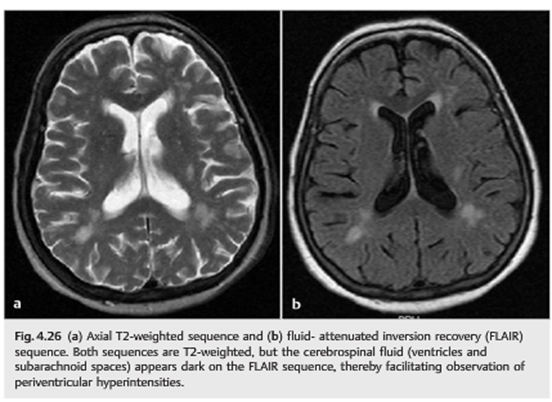
Because the ventricles are filled with CSF, a regular T2 sequence shows the ventricles and the subarachnoid space as very bright and does not allow for good evaluation of periventricular lesions, such as the white matter lesions from multiple sclerosis. A specific sequence called fluid-attenuated inversion recovery (FLAIR) allows transformation of the bright CSF signal into black signal, while maintaining the other characteristics of a T2-weighted image. FLAIR images are therefore “black CSF” T2-weighted images (▶Fig. 4.26).
Specific T2 sequences (gradient echo) also allow better visualization of blood products, such as hemosiderin. These sequences are particularly helpful when evaluating patients with cerebral vascular malformations, tumors, trauma, or infarctions.
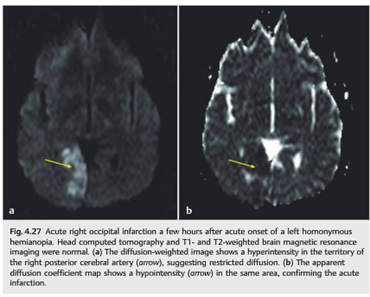
Diffusion-weighted images are ideal in detecting acute cerebral ischemia. They demonstrate restricted diffusion within hours of acute cerebral ischemia (while CT and other MRI sequences are often still normal) and should be obtained in all patients with acute neurologic deficits or when cerebral ischemia is suspected (▶Fig. 4.27).
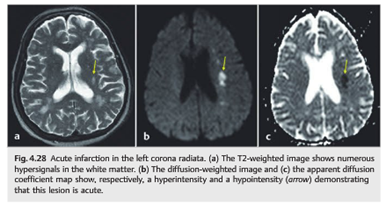
The appearance of lesions varies on diffusion-weighted images based on the time elapsed since the infarction. Old ischemic lesions do not show restricted diffusion, whereas acute ischemic lesions appear hyperintense on diffusion-weighted images and hypointense on the apparent diffusion coefficient (ADC) map (▶Fig. 4.28).
It is important to know which type of MRI to order. For example, with suspicion of cerebral infarction, a stroke protocol MRI of the brain should be ordered. This typically includes MRI without contrast (including sagittal T1-weighted sequence, axial T1-weighted sequence, axial FLAIR sequence, T2-weighted sequence, and often gradient echo to detect blood), MRI with diffusion weighted images (shows very acute infarctions), and MRI with magnetic resonance angiography (MRA) of the head (circle of Willis) and neck (extracranial cervical arteries).
In the case of optic neuropathy, MRI of the brain and orbits with contrast should be ordered. This includes regular MRI of the brain with contrast (including sagittal T1-weighted sequence, axial T1-weighted sequence, axial FLAIR sequence, and T1- weighted sequence with contrast) and dedicated orbital views (including axial and coronal T1-weighted sequence with and without fat suppression, as well as axial and coronal T1-weighted sequence with fat suppression and with contrast).
In the case of chiasmal syndrome, the examiner should order an MRI scan of the brain and orbits with contrast, with special attention to the pituitary gland. T1, T2, and T1 axial, coronal, and sagittal views of the sella turcica and pituitary gland with contrast should also be ordered.
In the case of cranial nerve deficit, the examiner should order an MRI scan of the brain with contrast, with special attention to the specific cranial nerve. Imaging should also include very thin axial and coronal cuts in T1, T2, and T1 with contrast, covering the anatomical course of the cranial nerve in question.
The following are good indications for MRI:
● Optic neuropathy
● Suspected optic nerve tumor
● Wooden foreign body
● Orbital apex or cavernous sinus syndrome
● Chiasmal syndrome
● Brain lesion
● Fungal sinusitis”1
Reference: 1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.