Questions:
8. What tests should be done in all patients over age 50 with transient or permanent diplopia?
9. What is the Silent Sinus Syndrome?
10. What is the Kearns-Sayre syndrome?
11. What are 5 mitochondrial diseases that can have ophthalmoplegia?
12. What are the features of Myotonic Dystrophy?
13. What are the features of Oculopharyngeal Dystrophy?
14. What 3 conditions other than paresis or restriction should be considered in any adult with new-onset transient or permanent ocular misalignment?
15. What may induce the myasthenia gravis or make it worse?
16. What is the mechanism of action of edrophonium?
17. What are the side effects of the Tensilon test?
18. What does the development of lid retraction in a patient with Myasthenia suggest?
19. What percent of patients presenting with purely ocular myasthenia will progress to develop generalized disease?
20. Does myasthenia gravis ever affect the pupils?
21. Does myasthenia gravis ever cause pain?
Questions of the Week: Diplopia 4 – Binocular Diplopia 2
Questions of the Week: Diplopia 3 Diagnosis of Binocular Diplopia 1
Questions:
1. What is the most common cause of unilateral proptosis?
2. What is the most common cause of bilateral proptosis?
3. Which is the most commonly involved extraocular muscle in thyroid eye disease?
4. What conditions should be considered in a patient with enlarged extraocular muscles?
5. On CT or MRI, which condition spares the insertions of the extraocular muscles, thyroid eye disease or idiopathic orbital inflammation (orbital pseudotumor)?
6. What 4 features differentiate idiopathic orbital inflammation (orbital pseudotumor) from thyroid eye disease?
7. When should a biopsy be done in a patient with presumed “myositis”?
Questions of the Week: Diplopia 2 – Assessment
Questions:
13. How is Bell phenomenon checked in normal patients?
14. When Bell’s phenomenon is preserved despite an upgaze paresis, where is the lesion?
15. What is the localizing value of abnormal eye movements that are overcome by oculocephalic maneuvers?
16. What is the usual symptom noted by a patient with convergence insufficiency?
17. A patient presents with a history of the onset of diplopia 3 weeks ago. What should be the first characteristic of the diplopia determined?
18. Your exam confirms that a patient has patient binocular diplopia, but on exam the extraocular movements appear full. What must be present?
19. Your exam confirms that a patient has patient binocular diplopia, but on exam the extraocular movements appear full. What tests will be helpful in demonstrating the misalignment?
20. What will the cross-cover test detect that the cover-uncover test will not detect?
21. When is a phoria pathologic and not physiologic?
22. Is the 3-step-test useful in horizontal or vertical binocular diplopia?
23. What reflex is involved in the 3rd step of the 3-step-test?
24. With the red Maddox rod placed between placed between a light source and the eye, what does the eye see?
25. Why would one perform a double Maddox Rod test?
26. When are the Hirschberg and Krimsky tests useful?
27. How is the Hirschberg test performed?
28. How is the Krimsky test performed?
29. In a comatose patient you observe dysconjugate horizontal eye movements when the head is rotated from side to side. What does this suggest?
Neuro-ophthalmology Questions of the Week: Diplopia1 – Basics
Questions:
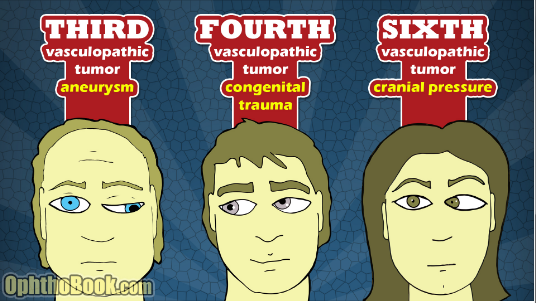
1. What 5 anatomical components of eye movement can cause binocular diplopia?
2. What holds the image steady during brief head movements?
3. What holds the image steady during sustained head movements?
4. What is Sherrington’s law?
5. What is Hering’s Law?
6. What 2 processes cause most incomitant strabismus?
7. What is the primary deviation in incomitant strabismus?
8. What is the secondary deviation in incomitant strabismus?
9. In incomitant strabismus, is the primary or secondary deviation larger?
10. Does a phoria or a tropia have more value in localizing the defect in a patient with new onset binocular diplopia
11. What is the difference between terms “ocular motor” and “oculomotor”?
12. What is the difference between ductions, versions and vergences?
13. What 3 techniques can help determine if an ocular misalignment is due to a restriction or paresis?
Cardinal features of superior oblique myokymia: An infrared oculography study
Recommended Reading
Question: What are the cardinal features of superior oblique myokymia?
Answer: There are 6 cardinal features of eye movement abnormality in superior oblique myokymia including:
1) involuntary intorsion and torsional oscillations;
2) episodic events lasting seconds;
3) worsening with infraduction and abduction positions that require activation of the superior oblique, and improvement with supraduction and adduction positions where the superior oblique is not activated;
4) overshooting of saccades on infraduction;
5) extorsion and diminished oscillations that were unmasked upon removal of a visual target, consistent with underlying weakness; and
6) improvement with membrane stabilizers used to treat neuropathic conditions. These features localized the lesion to the trochlear nerve, fascicle, or nucleus but not to the superior oblique muscle or neuromuscular junction.
Neuro-ophthalmology Question of the Week: Paraneoplastic Syndromes in Neuro-Ophthalmology
Question: When should an ophthalmologist consider the diagnosis of a paraneoplastic syndrome?
 2
2
Question with answers: When should an ophthalmologist consider the diagnosis of a paraneoplastic syndrome?
“In terms of afferent symptoms, an unexplained, painless, progressive vision loss is typical. With retinal involvement, there may be photopsias, night blindness, or ring scotomas. In the optic neuropathies, there is most commonly bilateral disc swelling often accompanied by vitritis. Efferent symptoms include myasthenic-like presentation or the presence of opsoclonus/myoclonus syndrome (OMS).”1
Neuro-ophthalmology Question of the Week: Neuro-ophthalmology Coma Eye Exam
Question:
Which of the following are correct for a patient?
1. The eyes of a patient in coma will be closed.
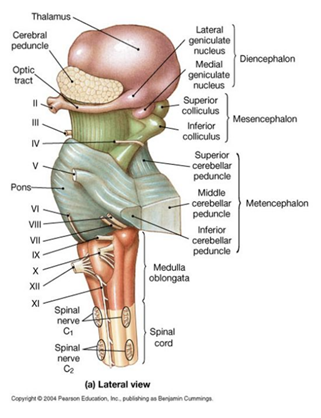
2. Because the pathways governing ocular motility traverse the entire brainstem, brainstem lesions will most often result in abnormal eye movements, and the lesion can be localized to the midbrain, pons, or medulla.
3. The presence of a dysconjugate ocular deviation in coma (horizontal, vertical, or oblique misalignment) often indicates a cranial nerve palsy or skew deviation.
4. Roving eye movements: slow ocular conjugate deviations in random directions indicate intact ocular motility function in the brainstem.
5. Periodic alternating (“ping-pong”) gaze: slow, repetitive, rhythmic, back-and-forth, horizontal conjugate eye movements indicates intact ocular motility function in the brainstem.
6. Normal vertical and horizontal oculocephalic reflexes indicate intact ocular motility function in the brainstem.
 1
1
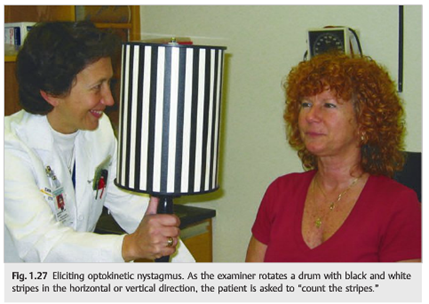
Neuro-ophthalmology Question of the Week: Optokinetic Testing
Question: In which of the following conditions is optokinetic stimulus testing useful?
1. Infantile nystagmus
2. Patients claiming complete blindness
3. Homonymous hemianopia
4. Internuclear ophthalmoplegia
5. Dorsal midbrain syndrome
6. Optic neuritis
 1
1
Neuro-ophthalmology Question of the Week: Emergency Department Evaluation of Diplopia
Question: Describe the appropriate steps to take in evaluating diplopia in the emergency department.
Neuro-ophthalmology Question of the Week: Ptosis, Miosis and Impaired Abduction
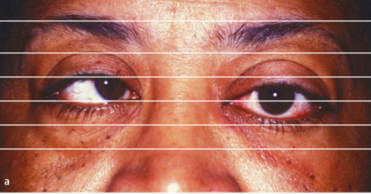
![]()
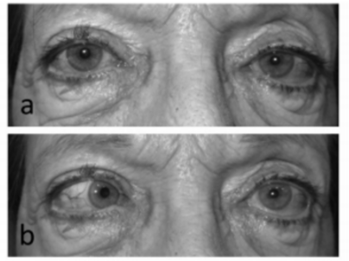
a. Primary position b. Left gaze 1
Question: Where is the lesion likely to be located?
1. Brain stem
2. Spinal cord
3. Left cavernous sinus
4. Left superior orbital fissure
5. Left orbit
