![]()
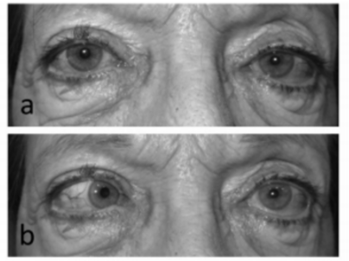
a. Primary position b. Left gaze 1
Question: Where is the lesion likely to be located?
1. Brain stem
2. Spinal cord
3. Left cavernous sinus
4. Left superior orbital fissure
5. Left orbit
Correct Answer:
- Left cavernous sinus
Explanation:
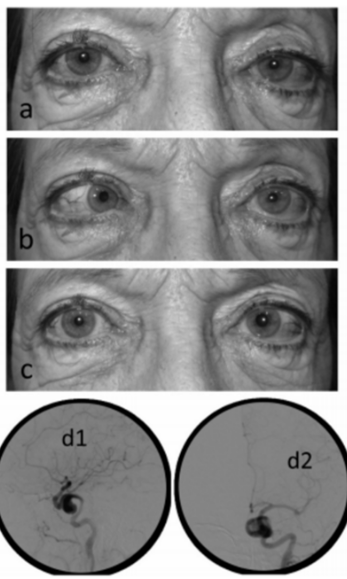
Figure 3. (a and b) Left eye VI palsy and Horner Syndrome.
(c) Apraclonidine 0.5% response after 30 min.
(d1 and d2) Frozen image of carotid cine-Angiography, d1 lateral and d2 frontal views, showing Intracavernous-carotid aneurysm.1
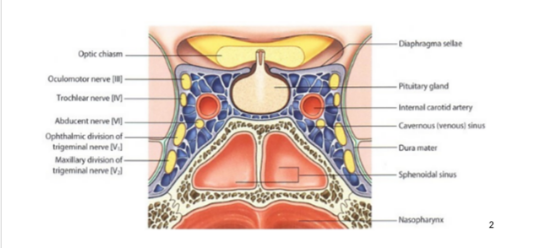
“The cavernous sinus is a structure that contains, in its lateral (meningeal) wall the oculomotor (IIIrd nerve), trochlear (IVth nerve) and the first two divisions of the trigeminal nerve. Inside the cavernous sinus, contains the abducens (VIth nerve) and the oculosympathetic nerve plexus around the internal carotid artery.
Isolated VIth nerve palsy or Horner Syndrome alone, has no localizing value per se, neuroimaging or pharmacological tests are necessary to determine the injury site.
The association of VIth nerve palsy with ipsilateral HS, described by Parkinson and named after him has a great localizing value, being the cavernous sinus the site of the lesion.
The sympathetic plexus and the VIth nerve attempt can be explained by the close anatomical relationship between these two elements inside the cavernous sinus. A single lesion may produce both deficits simultaneously.
The most frequent etiologies reported for Parkinson syndrome are; aneurism, invasive tumors, trauma, meningioma and giant cell arteritis.
In our small series of five cases we found two meningiomas, one carotid-cavernous aneurysm, one foreign body (bullet) and a squamous cell carcinoma as responsible for Parkinson syndrome. Neuroimaging (MRI, CT and Angiography) confirmed the initial clinical diagnostic showing cavernous sinus lesions in all our patients.
The use of Apraclonidine 0.5% has a great diagnostic value for HS but does not provide information about the level of the sympathetic pathway lesion. In our five cases helped to confirm the presence of sympathetic denervation (ipsilateral to the VI nerve deficit)”1
References:
- Sixth nerve palsy + ipsilateral Horner’s Syndrome = Parkinson’s Syndrome. Roberto N. Ebner RN, Ayerza DR, Aghetoni F. Saudi Journal of Ophthalmology (2015) 29, 63–66
- Cavernous Sinus Diagram http://educoma.com/dural-venous-sinuses-single-paired/
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.
To unsubscribe, reply to this email with “unsubscribe” as email topic or message content.
