Question: Describe the appropriate steps to take in evaluating diplopia in the emergency department.
_____________________________________________________
ED Concerns: aneurysm, giant cell arteritis, multiple sclerosis, myasthenia gravis, intraorbital or intracranial tumor, diabetic and other vasculopathic cranial nerve paresis
ED Evaluation:
1. Rule out monocular diplopia – not an emergency
A. Alternate Cover test – diplopia persists when one eye occluded = monocular diplopia
B. Pinhole test – have patient look at distant object through pinhole with eye with monocular diplopia and the other eye occluded.
a. Diplopia disappears = refractive error, poorly fit contact lens, corneal abnormalities, lid abnormalities, iris abnormalities, lens abnormalities, retinal abnormalities
– Arrange ophthalmology clinic follow-up
b. Diplopia persists = cerebral polyopia, psychogenic
– Arrange neuro-ophthalmology clinic follow-up
2. Binocular diplopia present
A. Confirm by questioning patient that images are not distorted or of different sizes, i.e. diplopia not due to metamorphopsia, or aniseikonia. – Arrange ophthalmology clinic follow-up.
B. Determine if diplopia is comitant or incomitant by measuring tropia in different positions of gaze.
a. Comitant misalignment
– Arrange strabismus clinic follow-up – not an emergency.
b. Incomitant misalignment – possible cranial nerve paresis, supranuclear palsy, oculomotor pathway lesion, restrictive disease, myasthenia gravis
– Intermittent diplopia in patient over age 50 Stat ESR, CRP, Platelets to rule-out giant cell arteritis
– Perform Ductions
➧ Normal Ductions rules-out restrictive process
➧ Abnormal Ductions
⏩ Determine if defect is supranuclear or infranuclear
⧫ Perform Doll’s Head Maneuver (oculocephalic reflex)
➤ If the oculocephalic reflex is normal (overcomes abnormal duction) = supranuclear cause – Obtain emergent brain MRI with and without contrast.
➤ If the oculocephalic reflex is abnormal = infranuclear cause
— Perform Forced Ductions
— Positive Forced Ductions = restrictive disease – Thyroid ophthalmopathy, Inflammation, Trauma, Orbital Tumors – Arrange oculoplastics ED consultation.
— Negative Forced Ductions rule-out cranial nerve paresis.
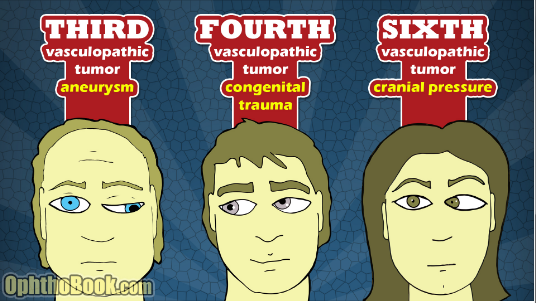
—Determine if pattern matches 3rd, 4th, 6th cranial nerve paresis or multiple cranial nerve paresis
—Horizontal tropia – observe adduction and abduction to determine which EOMs are affected
—Vertical tropia – perform Park’s 3 step test to determine which EOMs are affected.
– If pattern matches single or multiple cranial nerve paresis or Internuclear ophthalmoplegia obtain emergent orbit and brain MRI with and without contrast.
— If pattern matches 3rd nerve paresis add emergent CT angio or MR angio.
– If MRI, CTA, or MRA is positive obtain ED neurology/neurosurgery consultations.
– If neuroimaging negative – consider myasthenia gravis and vasculopathic cranial nerve palsy or paresis.
— Order Hemoglobin A1C and Myasthenia gravis adult antibody screening panel
— Arrange ED neurology consult
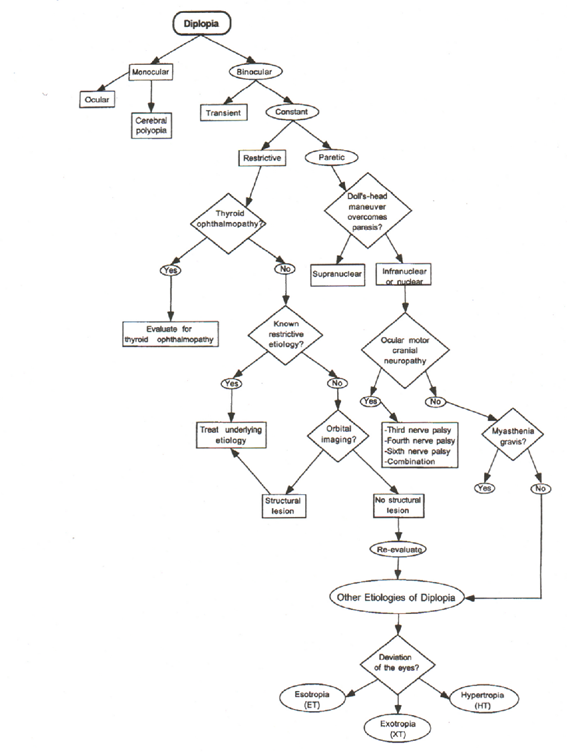
Diplopia Care Path
From: Clinical Pathways in Neuro-ophthalmology 2003
References:
1. OphthoBook. Root T. http://ophthobook.com/photos/eyepalsy-14-cranialnervepalsy.jpg
2. Clinical Decisions in Neuro-Ophthalmology, Burde RM, Savino PJ & Trobe JD. 3nd Edition. Mosby 2002
3. Clinical Pathways in Neuro-ophthalmology:An Evidence-Based Approach. Lee AC & Brazis PW. Thieme 2003
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.