Question: Describe the appropriate steps to take in evaluating monocular transient vision loss (TVL) in the emergency department.
Answer: ED Concerns: arteritic anterior ischemic optic neuropathy, embolic/thrombotic stroke, branch or central retinal artery occlusion, ocular ischemia, and angle closure glaucoma.
Monocular TLV without visual scintillations
- Age 50+ rule out GCA – obtain Stat ESR, CRP, CBC platelet count
- If these tests are negative but strong suspicion of GCA, consider systemic corticosteroids (discuss with on-call attending).
- GCA may present with TLV or diplopia.
- About 20% of GCA cases with vision loss have no systemic symptoms.4
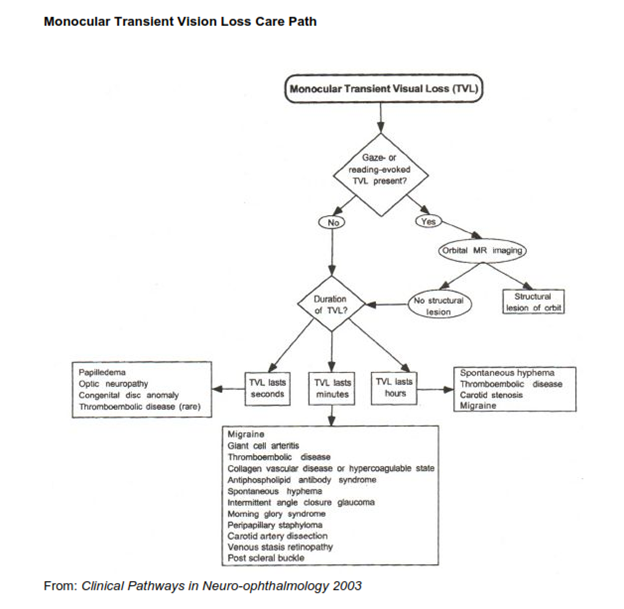
- TVL evoked by gaze or reading – obtain orbital MRI to rule-out intraorbital mass.
- History: onset with bright light exposure – rule out carotid artery disease and the ocular ischemia syndrome.
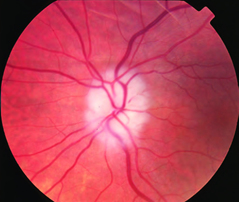
- Rule-out ocular cause: Retinal artery occlusion, recurrent hyphema, angle closure glaucoma, optic disc anomaly, papilledema, vein occlusion, or other optic neuropathy.
- Obtain diffusion-weighted MRI for all patients with TIAs including amaurosis fugax, and acute central or branch retinal artery occlusion.
Co-occurrence of Acute Retinal Artery Occlusion and Acute Ischemic Stroke-Diffusion-weighted MRI study. Lee J, et al. AJO. 2014:157(6):1231-1238
Transient Ischaemic Attacks: Mimics and Chameleons. Nadarajan V, et al. Pract Neurol. 2014;14(1):23-31.
Amaurosis Fugax – Transient monocular visual loss is often referred to as amaurosis fugax, irrespective of the cause. However, it is more accurate to reserve the term amaurosis fugax for episodes of transient monocular blindness resulting from ischemia. (Amaurosis fugax. An overview . Burde RM.J Clin Neuroophthalmol. Sep 1989;9(3):185-9.)
Rule-out likely sources of emboli and thrombi: obtain a medical consultation to rule out sources/causes of thromboembolism and thrombophilia.
Monocular TLV with visual scintillations
- Ocular migraine. True unilateral scintillations.
- Migraine with aura. Patients often fail to realize binocular hemifield (homonymous) visual field loss, e.g. the aura of migraine, affects the fields of both eyes. They usually localize the defect to the eye with the temporal field affected.
- If classic migraine symptoms are absent, consider conditions that can mimic migraine: occipital masses, SLE or chronic meningitis.3
TLV history, findings & likely cause
- TLV only in eccentric gaze positions or posture change or Valsalva maneuver
- Intraorbital mass, Idiopathic Intracranial Hypertension
- TLV with reading
- Intraorbital mass, Intermittent angle closure glaucoma
- TLV lasting only seconds
- Papilledema, Optic nerve sheath meningioma
- TLV lasting 2-30 minutes
- Very strongly suggests thromboembolic/ischemic disease
- TVL associated with bright light exposure
- Carotid artery disease and ocular ischemia syndrome
- TVL with pain
- Carotid artery dissection – 28% have TLV usually painful and often with Horner syndrome and may have contralateral motor or sensory symptoms.
References:
1. Clinical Decisions in Neuro-Ophthalmology, Burde RM, Savino PJ & Trobe JD. 3nd Edition. Mosby 2002
2. Clinical Pathways in Neuro-ophthalmology:An Evidence-Based Approach. Lee AC & Brazis PW. Thieme 2003
3. Migraine: mimics, borderlands and chameleons. Angus-Leppan H. Pract Neurol. 2013;13(5):308-18.
4. Giant cell arteritis: ophthalmic manifestations of a systemic disease. De Smit E, O’Sullivan E, Mackey DA, Hewitt AW. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2016:1-16
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.