Question: Describe the appropriate steps to take in evaluating binocular transient vision loss (BTVL) in the emergency department.
Concerns: intracranial ischemia (embolism, thrombus), GCA, SLE, , chronic meningitis. Most common = migraine
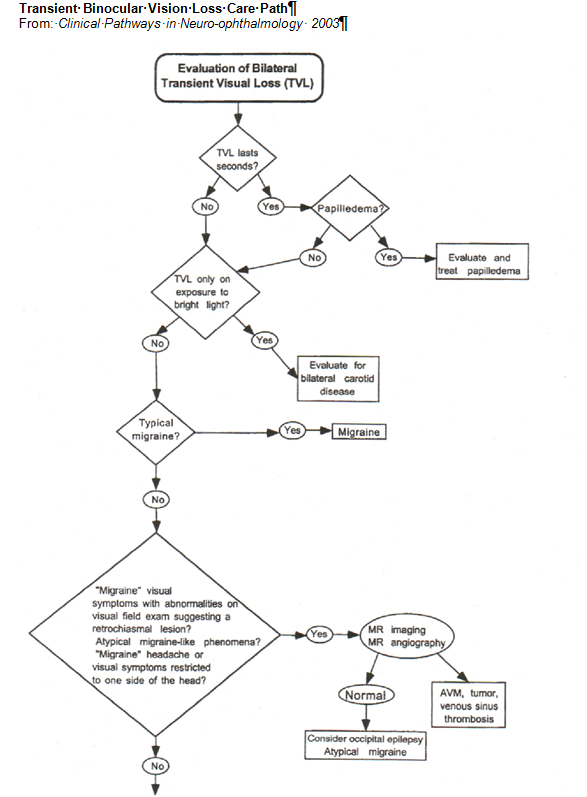
ED Evaluation of Binocular Transient Vision Loss
- Rule-out ocular cause – very unlikely for transient bilateral loss of vision
- If no ocular cause – Age 50+ rule out GCA
- obtain CBC ESR, CRP, CBC with platelet count
- If these tests are negative but strong suspicion of GCA, consider systemic corticosteroids (discuss with on-call attending).
- BTVL duration is seconds long – rule-out papilledema
- visual field loss suggesting retrochiasmal visual field loss or
- visual symptoms limited to one side (hemianopic)
- Consider conditions that can mimic migraine: occipital masses, SLE or chronic meningitis.3
- Obtain MRI/MRA to rule-out mass, AVM and sinus thrombosis
- MRI/MRA negative consider epilepsy or atypical migraine
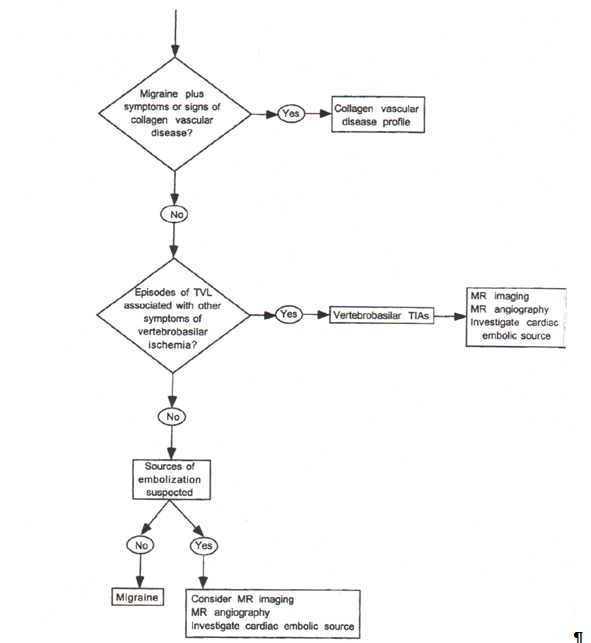
- Signs or symptoms of collagen vascular disease
- Obtain collagen vascular disease profile
- BTVL only exposure to bright light – rule-out bilateral carotid artery disease
- BTVL with typical migraine, diagnosis = migraine
- BTVL with “migraine” and with:
- BTVL consistent with TIA
- Obtain diffusion-weighted MRI for all patients with TIAs, an acute central or branch retinal artery occlusion.
- Co-occurrence of Acute Retinal Artery Occlusion and Acute Ischemic Stroke-Diffusion-weighted MRI study. Lee J, et al. AJO. 2014:157(6):1231-1238
- Transient Ischaemic Attacks: Mimics and Chameleons. Nadarajan V, et al. Pract Neurol. 2014;14(1):23-31.
- Rule-out likely sources of emboli and thrombi
- Obtain evaluation of carotid arteries and if negative a cardiac source.
- Obtain a medical consultation to rule out sources of thromboembolism and thrombophilia.
- Obtain diffusion-weighted MRI for all patients with TIAs, an acute central or branch retinal artery occlusion.
- BTVL consistent with TIA
References:
1. Clinical Decisions in Neuro-Ophthalmology, Burde RM, Savino PJ & Trobe JD. 3nd Edition. Mosby 2002
2. Clinical Pathways in Neuro-ophthalmology:An Evidence-Based Approach. Lee AC & Brazis PW. Thieme 2003
3. Migraine: mimics, borderlands and chameleons. Angus-Leppan H. Pract Neurol. 2013;13(5):308-18.
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.