Questions:
23. What is left-sided hemineglect?
24. How does one test for hemineglect?
25. What clinical signs are associated with left-sided hemineglect?
26. Where is the lesion in left-sided hemineglect?
27. What is topographagnosia?
28. What are the symptoms of topographagnosia?
29. What clinical signs are associated with topographagnosia?
30. Where is the lesion in topographagnosia?
Neuro-ophthalmology Illustrated Chapter 10 – Specific Disorders of Higher Cortical Function 4
Neuro-ophthalmology Illustrated Chapter 10 – Specific Disorders of Higher Cortical Function 3
Questions:
15. What is visual object agnosia?
16. How does one test for visual object agnosia?
17. What clinical signs are associated with object agnosia?
18. Where is the lesion in visual object agnosia?
19. What is optic aphasia?
20. How does one test for optic aphasia?
21. What clinical signs are associated with optic aphasia?
22. Where is the lesion in optic aphasia?
Neuro-ophthalmology Illustrated Chapter 10 – Specific Disorders of Higher Cortical Function 1
Questions:
1. What is the role of the inferior (ventral) or occipitotemporal pathway?
2. What is the role of the superior (dorsal) or occipitoparietal pathway?
3. What is alexia without agraphia?
4. How does one test for alexia without agraphia?
5. Where is the lesion in alexia without agraphia?
6. What clinical finding is associated with alexia without agraphia
Recommended Reading – 1. A ripping roller coaster ride & 2. Stroke
Recommended Reading – 1. A ripping roller coaster ride & 2. Stroke Due To Extracranial Internal Carotid Artery Dissection After Roller Coaster Rides In A 4-Year-Old Boy
A ripping roller coaster ride
David J. Blacker, Eelco F.M. Wijdicks
Neurology. 2003
NEUROIMAGES
ARTICLE
A 41-year-old woman presented with a right frontotemporal headache and drooping of the right eye. The previous day she rode a violent roller coaster ride twice (figure, left panel) and recalled vigorous jerking of her neck. Examination revealed a right Horner syndrome (figure, middle panel) with ptosis, meiosis, and no anhidrosis. Magnetic resonance angiography (figure, right panel) confirmed the diagnosis of right internal carotid artery dissection.
Figure. (A) The patient on the roller coaster ride. (B) Right Horner syndrome. (C) Magnetic resonance angiography confirmed the diagnosis of right internal carotid artery dissection.
Several other cases of carotid dissection have been reported related to amusement park equipment.
1 Roller coaster rides can generate force in excess of 4 “Gs,”1 which in combination with neck movements could potentially rip the carotid intima. Distension of the injured arterial wall compresses the adjacent sympathetic fibers,2 resulting in a Horner syndrome, which is typically without anhidrosis, in lesions above the bifurcation, where the fibers supplying the face leave to traverse with the external carotid artery.
References:
1. Braksiek R, Roberts D. Amusement park injuries and deaths. Ann Emerg Med . 2002; 39: 65–72.
2. Mokri B, Sundt T, Houser W, Piepgras D. Spontaneous dissection of the cervical internal carotid artery. Ann Neurol . 1986; 19: 126–138.
______________________________
Stroke Due To Extracranial Internal Carotid Artery Dissection After Roller Coaster Rides In A 4-Year-Old Boy
Amre Npuh, Daniel Vela-Duarte, Thomas Grobelny, George Hoganson, David Pasquale, Jose Biller.
Neurology. 2014; 82 (10 Supplement)
Abstract
OBJECTIVE: To describe the unusual association of stroke due to an extracranial right internal carotid artery (ICA) dissection following roller-coaster rides in a 4-year old boy. BACKGROUND: Strokes in children should prompt thorough investigations. Strokes associated with roller-coaster rides are unusual.
DESIGN/METHODS: A previously healthy 4-year-old boy frequented many roller coasters with his parents while on vacation at an out of state amusement park. On the flight home the following day, his parents noticed a left facial droop. Upon landing, he was unable to walk due to left sided weakness, prompting immediate evaluation. Magnetic resonance imaging (MRI) of the brain showed an acute right middle cerebral artery (MCA) territory infarction. Magnetic resonance angiography (MRA) showed right M1CA occlusion. Catheter cerebral angiogram performed one week later demonstrated an extracranial right ICA dissection. Transthoracic echocardiogram, extensive hypercoagulable panel, serum autoimmune and inflammatory markers and cerebrospinal fluid (CSF) analysis were unremarkable. Dermatoloical evaluation showed no evidence of connective tissue disease. He received low-dose aspirin.
RESULTS: Neurological function remained stable during his hospital stay, and on a 3 month follow-up he exhibited only mild residual left spastic hemiparesis.
CONCLUSIONS: To our knowledge this is the youngest patient with stroke secondary to ICA dissection following roller-coaster rides. Although the exact mechanism of injury leading to ICA dissection in the setting of sudden linear acceleration, deceleration and rotational forces such as those experienced while riding a roller coaster is not fully understood, these injuries have been attributed to brief sustained excessive gravitational forces likely augmented among predisposed individuals. Children may be at higher risk due to the immature anatomy of their cervical spine. Alterations to roller coaster ride dynamics and use of head restraints may be a reasonable first approach to lower this potential, albeit unusual risk.
Neuro-ophthalmology Questions of the Week: Terms – Disorders of Higher Cortical Function
Questions:
1. What are the names and functions of the 2 visual higher cortical function processing streams?
2. What are the findings in a patient with alexia without agraphia?
3. Where is the lesion in alexia without agraphia?
4. What is prosopagnosia?
5. What is visual object agnosia?
6. What is optic aphasia?
7. What is topographagnosia?
8. What is akinetopsia?
9. What is simultagnosia?
10. What is ocular apraxia?
Neuro-ophthalmology Question of the Week: Neuro-ophthalmology Coma Eye Exam
Question:
Which of the following are correct for a patient?
1. The eyes of a patient in coma will be closed.
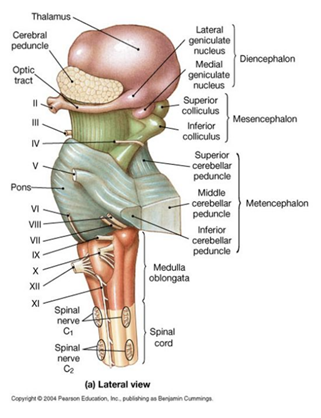
2. Because the pathways governing ocular motility traverse the entire brainstem, brainstem lesions will most often result in abnormal eye movements, and the lesion can be localized to the midbrain, pons, or medulla.
3. The presence of a dysconjugate ocular deviation in coma (horizontal, vertical, or oblique misalignment) often indicates a cranial nerve palsy or skew deviation.
4. Roving eye movements: slow ocular conjugate deviations in random directions indicate intact ocular motility function in the brainstem.
5. Periodic alternating (“ping-pong”) gaze: slow, repetitive, rhythmic, back-and-forth, horizontal conjugate eye movements indicates intact ocular motility function in the brainstem.
6. Normal vertical and horizontal oculocephalic reflexes indicate intact ocular motility function in the brainstem.
 1
1
Neuro-ophthalmology Question of the Week: Ptosis, Miosis and Impaired Abduction
![]()
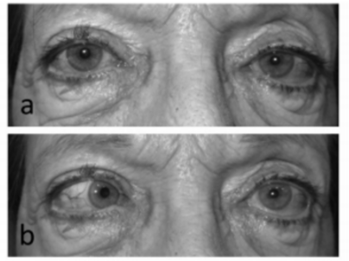
a. Primary position b. Left gaze 1
Question: Where is the lesion likely to be located?
1. Brain stem
2. Spinal cord
3. Left cavernous sinus
4. Left superior orbital fissure
5. Left orbit