Questions:
23. What is left-sided hemineglect?
24. How does one test for hemineglect?
25. What clinical signs are associated with left-sided hemineglect?
26. Where is the lesion in left-sided hemineglect?
27. What is topographagnosia?
28. What are the symptoms of topographagnosia?
29. What clinical signs are associated with topographagnosia?
30. Where is the lesion in topographagnosia?
____________________________________________________
Questions with answers:
23. What is left-sided hemineglect?
It is the Higher Cortical Disorder in which a deficit in attention to and awareness of one side of space is observed. It is defined by the inability of a person to process and perceive stimuli on one side of the body or environment, where that inability is not due to a lack of sensation. It results most commonly from strokes and brain unilateral injury to the right cerebral hemisphere, with rates in the critical stage of up to 80% causing visual neglect of the left-hand side of space. Neglect is often produced by massive strokes in the medial cerebral artery region and is variegated, so that most sufferers do not exhibit all of the syndrome traits. Right-sided hemineglect is extremely rare.
24. How does one test for hemineglect?
Draw a line a few inches long on a piece of paper and ask the patient point to the midpoint of the line. Patients exhibiting left-sided neglect will exhibit a rightward deviation of the line’s true midpoint. Visual neglect can also be assessed by having the patient draw a copy of a picture with which they are presented. They may neglect the entire contralesional side of the picture or only note a few details. If asked to draw an individual object, the patient man not draw the contralesional side of that object or that side will have few details.
25. What clinical signs are associated with left-sided hemineglect?
Inattention, Left sensorimotor hemiparesis
26. Where is the lesion in left-sided hemineglect?
The right inferior parietal lobe, the frontal cortex, and the thalamus.
27. What is topographagnosia?
It is the Higher Cortical Disorder in which the patient is unable to identify familiar landmarks and buildings.
28. What are the symptoms of topographagnosia?
The patient will get lost in familiar surroundings.
29. What clinical signs are associated with topographagnosia?Prosopagnosia and Achromatopsia
30. Where is the lesion in topographagnosia?
Right inferior occipitotemporal lobes
The information below is from Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Thieme
10 Disorders of Higher Cortical Function
Unlike the anterior visual and geniculocalcarine pathways that deliver basic visual information from the eyes to the occipital cortex, association cortical visual areas (higher cortical areas) perform the more complex interpretation of visual information. Many of the syndromes of higher cortical dysfunction are secondary to a disconnection of the flow of visual information between the striate cortex and other cortical regions. When these areas are damaged, visual processing is abnormal despite often normal visual acuity and visual fields.
This chapter focuses on some of the main visual disorders of higher cortical function, particularly their clinical and radiologic findings and causes, commonly encountered in neuro-ophthalmology.
10.1 Classification
Disorders of higher cortical function are often grouped into two processing streams. The first stream, the inferior (ventral) or occipitotemporal pathway for object recognition, extends from below the calcarine fissure into the adjacent temporal lobe. It facilitates object recognition and color perception. Disorders here include achromatopsia, prosopagnosia, alexia, and topographagnosia.
The second stream, the superior (dorsal) or occipitoparietal pathway for object localization extends from the upper bank of the calcarine fissure into the adjacent parietal lobe. It processes visuospatial attributes, including location and motion. Disorders here include akinetopsia, Balint syndrome (simultagnosia, ocular apraxia, and optic ataxia), and hemineglect.
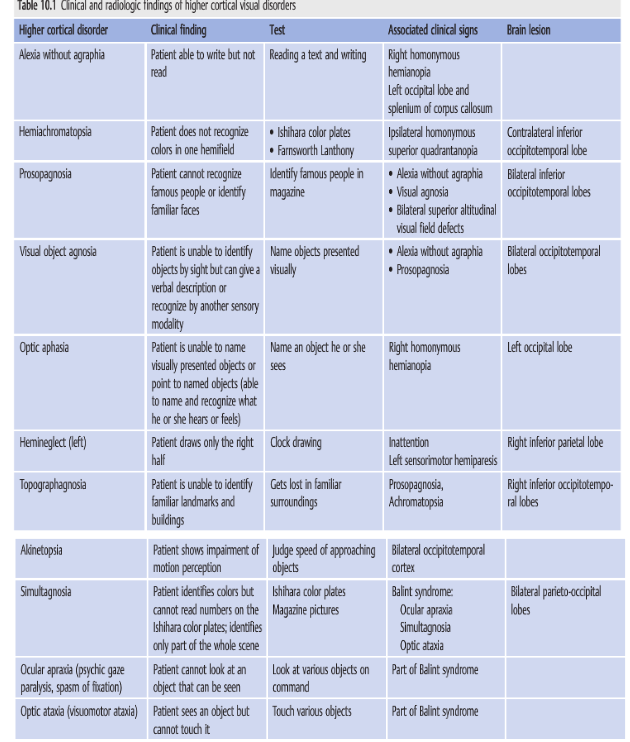
▶Table 10.1 lists the clinical findings, recommended tests, associated clinical signs, and lesions associated with these higher cortical disorders.
Reference: 1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Thieme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.