Question: What are 5 categories of symptoms that help differentiate the 3 most common causes of binocular transient vision loss (migraine visual aura, occipital transient ischemic attacks, and occipital seizures)?
 1
1
Question: What are 5 categories of symptoms that help differentiate the 3 most common causes of binocular transient vision loss (migraine visual aura, occipital transient ischemic attacks, and occipital seizures)?
 1
1
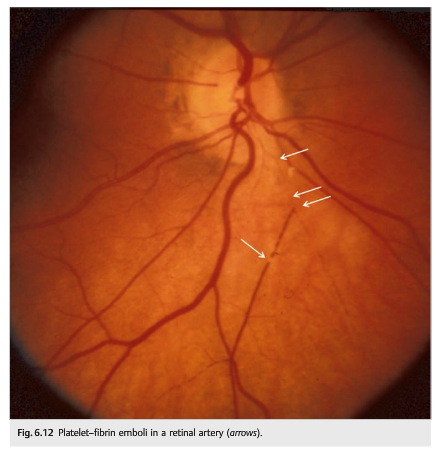
Questions:
1. What should be done immediately when a patient presents with a recent vascular TMVL?
2. What should be done emergently in the presence of an acute central retinal artery or branch retinal artery occlusion?
3. What is the chance and timeline of stroke after TMVL in the presence of ipsilateral atheromatous internal carotid stenosis ≥50%?
4. What is the yearly risk of vascular death (myocardial infarction) in patients with TMVL and atheromatous disease?
 1
1
Neuro-ophthalmology Question of the Week: Transient Monocular Vision Loss Categories
Question: What are the three main categories of transient monocular vision loss?
 1
1
Questions:
1. What is the preferred term for abrupt and temporary visual loss in one eye?
2. What is the most common cause of transient monocular vision loss?
3. What is amaurosis fugax?
 1
1
Question: What 3 historical factors can help establish that a transient loss of vision reported to be unilateral by the patient is consistent with the visual aura of migraine?
 1
1
Questions: Transient monocular vision loss with:
1. Headache, scalp tenderness, jaw claudication, and diplopia suggest?
2. Eye or brow pain suggests?
3. Neck pain suggests?
4. Ipsilateral Horner syndrome suggests?
5. Simultaneous contralateral hemisensory or motor findings suggests?
6. Presyncope suggests?
7. When moving the eye suggests?
8. Blurry vision when reading suggests?

Question: Which of the following are correct?
1. If visual acuity can be improved by the patient looking through a pinhole, the problem is refractive or ocular, not neurologic in origin.
2. Reduction in the saturation or brightness of colors may be an early sign of optic nerve disease.
3. A relative afferent pupillary defect ipsilateral to visual loss indicates an optic neuropathy or severe retinal disease (in which case the retina looks abnormal on funduscopic examination).
4. If nonorganic visual loss is suspected, normal stereovision indicates 20/20 visual acuity in both eyes.
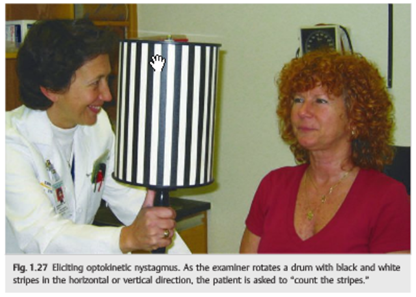
5. A positive response to the optokinetic nystagmus stimulus indicates a visual acuity of at least 20/400 in the eye tested.
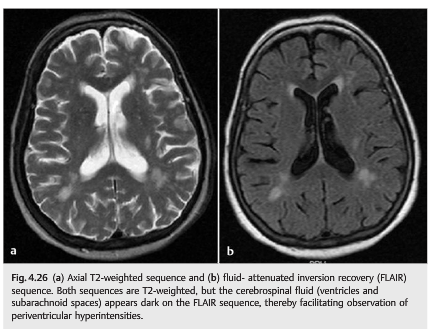
Question: Which of the following are correct?
1. Fat is hyperintense on T1.
2. Vitreous is hyperintense on T1.
3. CSF is hyperintense on T1.
4. Subacute blood is hyperintense on T1.
5. Fat is hypointense on T2.
6. Vitreous is hypointense on T2.
7. CSF is hypointense on T2.
8. Diffusion-weighted images are ideal in detecting acute cerebral ischemia.
9. T2 gradient echo allows better visualization of blood products, such as hemosiderin.
Question: On CT which of the following are isodense, hypodense, hyperdense, or enhance on contrast?
1 Acute clot in a large vessel
2 Blood vessels
3 Bone
4 Breakdown of the normal blood-brain barrier
5 Calcium
6 Edema
7 Fat
8 Fresh blood
9 Infarction
10 Inflammatory lesions
11 Necrosis
12 Neoplasms
13 Normal brain

Question: Which of the following are good indications for CT and which for MRI?
1 Bone lesions
2 Brain lesions
3 Chiasmal syndrome
4 Fungal sinusitis
5 Infectious or noninfectious orbital inflammation
6 Lacrimal gland lesions
7 Lesions that may contain calcium
8 Ocular trauma to rule out a foreign body
9 Optic neuropathy
10 Orbital apex or cavernous sinus syndrome
11 Orbital trauma
12 Preoperative imaging for orbital disease when imaging of the facial sinuses is very important
13 Suspected optic nerve tumor
14 Wooden foreign body