Questions:
1. What is the preferred term for abrupt and temporary visual loss in one eye?
2. What is the most common cause of transient monocular vision loss?
3. What is amaurosis fugax?
 1
1
Questions with answers:
1. What is the preferred term for abrupt and temporary visual loss in one eye? Transient monocular visual loss
2. What is the most common cause of transient monocular vision loss?
Transient ocular ischemia
3. What is amaurosis fugax?
Transient ocular ischemia
Explanation:“6.2 Transient Monocular Visual Loss
Transient monocular visual loss (TMVL) is the preferred term for abrupt and temporary visual loss in one eye. TMVL most often results from transient ocular ischemia (so-called amaurosis fugax), but it may also result from other mechanisms such as disc edema and numerous ocular diseases. See the discussion in Chapter 5.
6.2.1 Differential Diagnosis
TMVL can be vascular (transient ischemia in the territories of the ophthalmic artery, central retinal artery and its branches, posterior ciliary arteries, or central retinal vein), can be ocular in origin (such as from dry eyes or attacks of angle closure glaucoma), or can result from optic nerve head anomalies.
An orbital mass may produce gaze-evoked episodes of TMVL. The examination may be normal between episodes when the mass is relatively small. Movements of the eye result in stretching of the optic nerve and intermittent compression of the nerve or of its blood supply, with resulting transient loss of vision.
Eyes with a narrow anterior chamber angle may have episodes of angle closure glaucoma resolving spontaneously. During such episodes, the intraocular pressure is elevated, and patients complain of painful transient monocular blurry vision with the perception of halos around lights.
Patients with dry eyes often complain of fluctuation of vision, especially while reading.
Pearls
Transient visual obscurations (TVOs) are characterized by brief blackouts or “gray-outs” of vision and are precipitated by changes in posture, such as bending over. They usually indicate underlying optic nerve head edema or optic nerve anomalies causing high tissue pressure at the optic nerve head. Although disc edema results from a variety of disorders, the most likely cause of TVOs is papilledema from raised intracranial pressure.
6.2.2 Patient Evaluation
The clinical history and a detailed ocular examination help determine the mechanism of the TMVL.
Among the first things to ask the patient about are the onset and duration of TMVL. The answers can help determine the cause. For example, retinal emboli produce a very sudden TMVL, lasting from 1 to 4minutes. TMVL as a result of ocular hypoperfusion would be progressive, at least 5 to 10 minutes, and be precipitated by standing up or looking at bright lights. Venous congestion causes a progressive loss, lasting at least 10 to 20minutes. TVOs from optic nerve head anomalies are very brief, lasting only a few seconds, and are precipitated by bending over or by Valsalva maneuvers.
Accompanying manifestations helpful in determining the mechanism of TMVL include the following:
- Headache, scalp tenderness, jaw claudication, and diplopia: giant cell arteritis
- Eye or brow pain: intermittent angle closure glaucoma or giant cell arteritis
- Neck pain: cervical carotid artery dissection
- Ipsilateral Horner syndrome: carotid artery dissection
- Simultaneous contralateral hemisensory or motor findings: ipsilateral carotid artery stenosis
- Presyncope: systemic hypotension or a hyperviscosity syndrome
- TMVL when moving the eye: orbital mass
- Blurry vision when reading: dry eyes
The ocular examination can help to rule out local causes of TMVL and detect retinal emboli, retinal ischemia, venous stasis retinopathy, or evidence of optic nerve ischemia.
Eyes with a narrow anterior chamber angle may have episodes of angle closure glaucoma resolving spontaneously (▶Fig. 6.5).
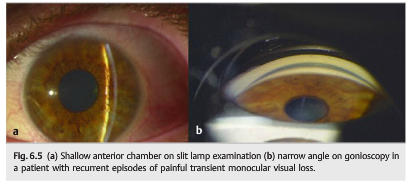
During such episodes, the intraocular pressure is elevated, and patients complain of painful transient monocular blurry vision with the perception of halos around lights.
6.2.3 Vascular TMVL
Vascular TMVL is the most common and perhaps most important ophthalmologic symptom of carotid occlusive disease (see Chapter 20). Patients with vascular TMVL complain of isolated or recurrent episodes of acute, monocular loss of vision that may be partial or complete.
▶Fig. 6.6 shows the blood supply of the eyes and the orbits.
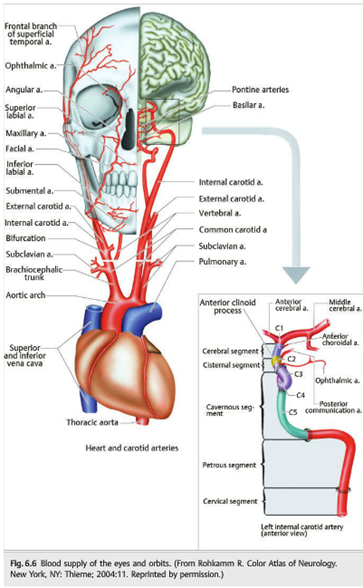
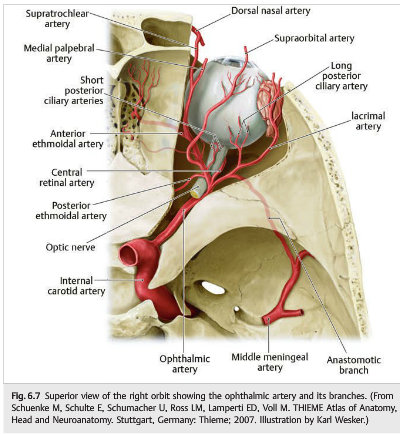
The main blood supply to the eye and orbital contents comes from the ophthalmic artery, a branch of the internal carotid artery (▶Fig. 6.7).
Any vascular disease involving the arteries between the heart and the ophthalmic artery may result in ocular ischemia and visual loss.
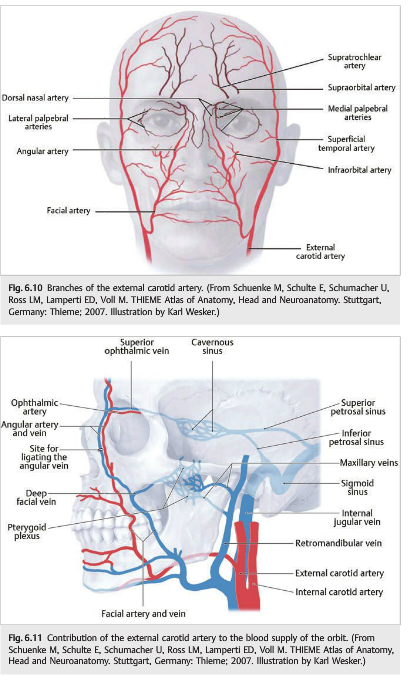
The external carotid artery and its branches also contribute to the vascularization of the eye and orbital contents. In cases of internal carotid artery stenosis or occlusion, the entire ocular vascularization may originate from the external carotid artery. In this situation, there may be a steal phenomenon from the eye to the brain, and the flow may be reversed in the ophthalmic artery so that most of the blood flow contributes to the vascularization of the ipsilateral cerebral hemisphere.
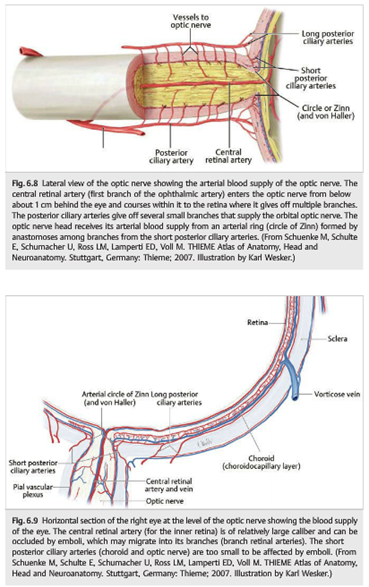
Branches of the ophthalmic artery (▶Fig. 6.8 and ▶Fig. 6.9) include the central retinal artery to the inner retina; the short posterior ciliary arteries to the choroid and optic nerve; the long posterior ciliary arteries to the ciliary body and iris; and the anterior ciliary arteries, which arise from the vessels of the rectus muscles. Occlusion of the ophthalmic artery results in complete ocular ischemia, whereas occlusion of the central retinal artery results in retinal ischemia.
Pearls
The external carotid artery is important for collateral circulation for the orbit and for the brain when there is severe occlusive disease of the internal carotid artery (, ▶Fig. 6.10, and ▶Fig. 6.11).
Mechanisms of Vascular TMVL
The mechanisms of vascular TMVL are emboli, hypoperfusion of the eye (hemodynamic TMVL), vasculitis (usually giant cell arteritis), arterial vasospasm (central retinal artery), and venous congestion (central retinal vein).
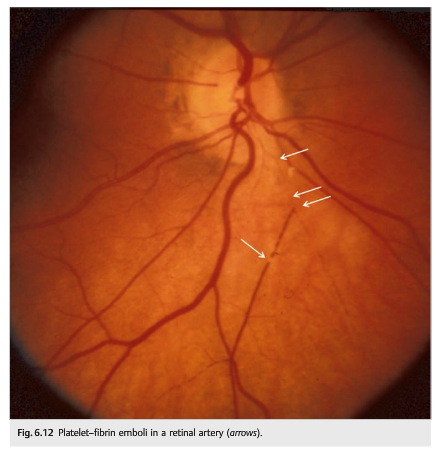
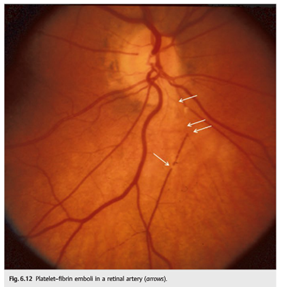
- Emboli into the retinal circulation (▶Fig. 6.12, ▶Fig. 6.13, and ▶Fig. 6.14) (central and branch retinal arteries) most often result from lesions of the common or internal carotid arteries that embolize material to the retinal circulation. With emboli, most commonly a black or dark shade spreads across the visual field of the affected eye, disappearing after a few minutes. Occasionally, emboli may be observed ophthalmoscopically as they pass through the retinal arterioles.


Pearls
Emboli (in the central retinal artery or the ophthalmic artery) represent the most common cause of transient or permanent retinal ischemia, which should warrant an immediate workup looking for a source of emboli. Carotid disease is the most common cause of retinal ischemia.”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.