Questions:
38. What is ocular apraxia?
39. How does one test for ocular apraxia?
40. What clinical signs are associated with ocular apraxia?
41. What is optic ataxia (visuomotor ataxia)?
42. How does one test for optic ataxia?
43. What clinical signs are associated with optic ataxia?
____________________________________________________
Questions with answers:
38. What is ocular apraxia?
It is the Higher Cortical Disorder in which the patient cannot look at a specific object that can be seen. (psychic gaze paralysis, spasm of fixation).
39. How does one test for ocular apraxia?
Ask the patient to look from one object to another. Typically head thrusts are used to compensate for their inability to initiate horizontal eye movements away from the straight-ahead gaze position. Typically, vertical eye movements are unaffected.
40. What clinical signs are associated with ocular apraxia?
Is a part of Balint syndrome: Ocular apraxia, Simultagnosia, Optic ataxia
41. What is optic ataxia (visuomotor ataxia)?
It is the Higher Cortical Disorder in which the patient sees an object but cannot touch it.
42. How does one test for optic ataxia?
Ask the patient to touch various objects.
43. What clinical signs are associated with optic ataxia?
Is a part of Balint syndrome: Ocular apraxia, Simultagnosia, Optic ataxia
____________________________________________________
The information below is from Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Thieme
10 Disorders of Higher Cortical Function
Unlike the anterior visual and geniculocalcarine pathways that deliver basic visual information from the eyes to the occipital cortex, association cortical visual areas (higher cortical areas) perform the more complex interpretation of visual information. Many of the syndromes of higher cortical dysfunction are secondary to a disconnection of the flow of visual information between the striate cortex and other cortical regions. When these areas are damaged, visual processing is abnormal despite often normal visual acuity and visual fields.
This chapter focuses on some of the main visual disorders of higher cortical function, particularly their clinical and radiologic findings and causes, commonly encountered in neuro-ophthalmology.
10.1 Classification
Disorders of higher cortical function are often grouped into two processing streams. The first stream, the inferior (ventral) or occipitotemporal pathway for object recognition, extends from below the calcarine fissure into the adjacent temporal lobe. It facilitates object recognition and color perception. Disorders here include achromatopsia, prosopagnosia, alexia, and topographagnosia.
The second stream, the superior (dorsal) or occipitoparietal pathway for object localization extends from the upper bank of the calcarine fissure into the adjacent parietal lobe. It processes visuospatial attributes, including location and motion. Disorders here include akinetopsia, Balint syndrome (simultagnosia, ocular apraxia, and optic ataxia), and hemineglect.
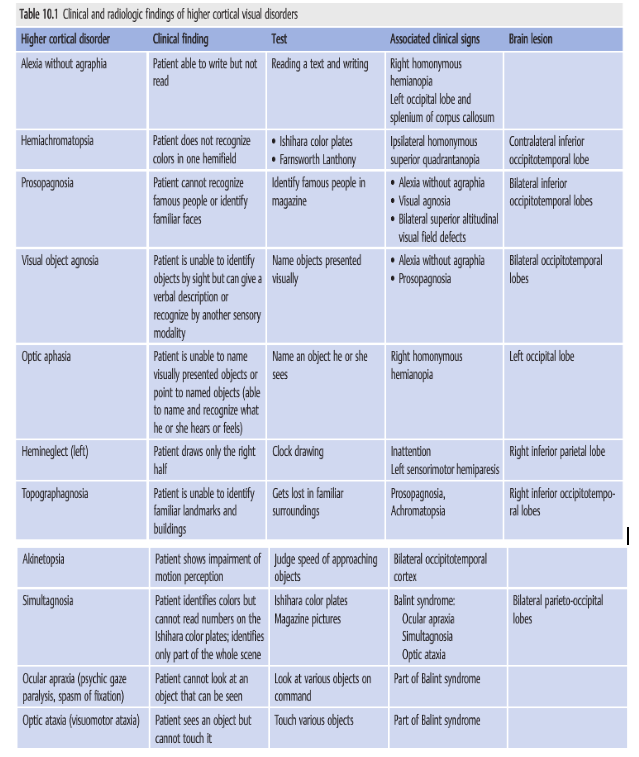
▶Table 10.1 lists the clinical findings, recommended tests, associated clinical signs, and lesions associated with these higher cortical disorders.
Reference: 1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Thieme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.