Questions:
1. What is the orbital syndrome?
2. What are the common features of the orbital syndrome?
3. What is the most common cause of unilateral or bilateral proptosis?
4. What should be suspected if there is globe displacement with proptosis?
5. Do brain CT and MRI often miss orbital processes?
____________________________________________________
Questions with answers:
1. What is the orbital syndrome?
An acute or subacute disorder involving the structures in the orbit. There are a number of specific syndromes that involve the orbit.
2. What are the common features of the orbital syndromes?
1. Proptosis
2. Eyelid malposition (Retraction, Ptosis)
3. Ocular pulsations or orbital bruit
4. Vision loss (optic neuropathy from compression, infiltration, ischemia, elevated intraocular pressure, venous stasis causing retinal hemorrhages, macular edema, serous retinal detachment)
5. Diplopia (extraocular muscle restriction from, venous engorgement, mechanical limitation secondary to mass effect, cranial neuropathy (secondary to nerve ischemia or direct compression)
6. Enophthalmos rarely (secondary to scarring with tissue retraction or bony orbital wall destruction)
3. What is the most common cause of unilateral or bilateral proptosis?
The most common cause of unilateral or bilateral proptosis is thyroid orbitopathy.
4. What should be suspected if there is globe displacement with proptosis?
Orbital tumors often produce proptosis with displacement of the globe.
5. Do brain CT and MRI often miss orbital processes?
Yes, brain neuroimaging often misses orbital processes. Orbital protocols for CT and MRI are necessary.
The information below is from Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
14 Orbital Syndrome
Orbital disorders usually manifest with symptoms and signs that include proptosis, periocular swelling, decreased vision, and diplopia.
14.1 Clinical Anatomy of the Orbit
All orbital structures can be involved in orbital lesions (▶Fig. 14.1). Because the orbit is an enclosed space surrounded by bones, any orbital process will result in proptosis (exophthalmos).
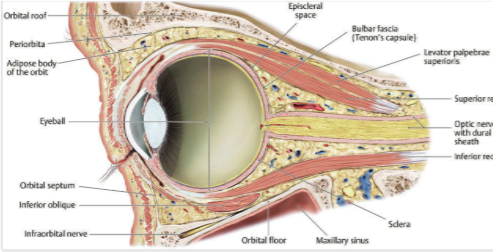
Fig.14.1 Anatomy of the orbit (sagittal view through the eye and the optic canal). (From Schünke M, Schulte E, Schumacher U,Rossa LM, Lamperti ED, Voll M. THIEME Atlas of Anatomy, Head and neuroanatomy. Stuttgart, Germany: Thieme;2007. Illustration by Karl Wesker.)
14.2 Causes of Acute or Subacute Orbital Syndrome
Acute orbital syndromes are most often vascular or inflammatory, whereas subacute presentations are most likely secondary to tumors.
Vascular abnormalities
● Carotid-cavernous sinus fistula
● Cavernous sinus thrombosis
● Superior ophthalmic vein thrombosis
● Orbital varix
● Orbital arteriovenous malformation
Inflammatory processes
● Infectious
○ Bacterial orbital cellulitis
○ Fungal infections
○ Orbital tuberculosis
● Noninfectious
○ Thyroid-related orbitopathy
○ Idiopathic orbital inflammation (inflammatory orbital pseudotumor)
○ Immunoglobulin G4 (IgG4) related disease
○ Sarcoidosis
○ Wegener granulomatosis
○ Giant cell arteritis
○ Polyarteritis nodosa
Tumors (only the most classic tumors in each age group are listed, in order of decreasing frequency)
● Primary
○ Adults
– Cavernous hemangioma
– Lymphangioma
– Schwannoma
– Lymphoma
– Optic nerve sheath meningioma
○ Children
– Rhabdomyosarcoma
– Lymphangioma
– Capillary hemangioma
– Optic nerve glioma
– Cysts, including mucocele
● Secondary/invasive
○ Sinonasal tumors
○ Brain tumors
○ Perineural spread of cutaneous tumors
● Metastatic
○ Adults
– Breast carcinoma
– Bronchogenic carcinoma
– Prostate carcinoma
○ Children
– Neuroblastoma
– Leukemia
Trauma
● Orbital wall fractures
● Retrobulbar hematoma
The clinical examination may help further differentiate among the possible etiologies, but imaging studies are imperative to ascertain the ultimate diagnosis. In the absence of diagnostic imaging findings, tissue biopsy is usually the next step in determining the cause of an orbital syndrome.
14.3 Features of Orbital Syndrom
The following symptoms and signs can reveal an orbitopathy:
● Proptosis (exophthalmos)
● Eyelid malposition
○ Retraction
○ Ptosis
● Globe displacement
● Ocular pulsations or orbital bruit
● Vision loss
○ Optic neuropathy from– compression
– infiltration
– ischemia
– elevated intraocular pressure
○ Venous stasis causing
– retinal hemorrhages
– macular edema
– serous retinal detachment
● Diplopia
○ Extraocular muscle restriction
– venous engorgement
– mechanical limitation secondary to mass effect
○ Cranial neuropathy (secondary to nerve ischemia or direct compression)
● Enophthalmos rarely (secondary to scarring with tissue retraction or bony orbital wall destruction)
14.3.1 Causes of Proptosis
Orbital space occupying lesions induce proptosis:
● Thyroid eye disease
● Orbital tumors
● Orbital inflammatory pseudotumor
● Orbital infection (cellulitis)
● Orbital vascular malformations
○ Arteriovenous malformations
○ Orbital varix
● Orbital venous congestion
○ Cavernous sinus fistula
○ Cavernous sinus thrombosis
○ Superior orbital vein thrombosis
○ Orbital hemorrhage
● Bony deformations of the orbit
○ Fibrous dysplasia
○ Sphenoid wing hypoplasia
● Trauma to the orbit
● Pseucoproptosis
○ High myopia
○ Racial (common in blacks)
Pearls
The most common cause of unilateral or bilateral proptosis is thyroid eye disease (▶Fig. 14.2).
Orbital tumors often produce proptosis with displacement of the globe (▶Fig. 14.3).
Orbital metastases from breast cancer are classically associated with atrophy of fat, resulting in enophthalmos rather than proptosis (exophthalmos) (▶Fig. 14.4).
14.4 Evaluation of a Patient with Orbital Syndrome
Because of the risk of visual loss, patients with suspected orbital syndrome must be evaluated urgently.
● Clinical:
○ Unilateral or bilateral
○Tempo of onset and duration of symptoms
○ History of trauma
○ Pain
○ Prognostic:
– Visual loss
– Elevated intraocular pressure
● Orbital imaging:
○ Computed tomography (CT) of the orbits with contrast
○ Magnetic resonance imaging (MRI) of the orbits with fat suppression and contrast
○ Orbital ultrasound (to detect enlarged extraocular muscles and superior ophthalmic vein)
● Orbital biopsy often necessary
An orbital syndrome is suspected clinically and is confirmed by imaging of the orbits with contrast (CT or MRI). Brain imaging often misses orbital processes. Orbital biopsy is often necessary.