Questions:
1. What is the classic tetrad of narcolepsy?
2. What is palinopsia?
3. What is polyopia?
4. What is the Alice in Wonderland syndrome?
5. What is visual allesthesia?
6. What is the Riddoch Phenomenon?
7. What is Blindsight?
8. What is Residual Vision?
9. What 6 conditions are associated oscillopsia?
10. What is the Anton Syndrome?
__________________________________________
Questions with answers:
1. What is the classic tetrad of narcolepsy?
– 1. Cataplexy (transient loss of muscle tone)
– 2. Sleep paralysis (inability to move when the patient first wakes up)
– 3. Sleep attacks (overwhelming sense of fatigue causing the patient to fall asleep for 10 to 30 minutes)
– 4. Hypnogogic (entering sleep) and hypnopompic (awakening) hallucinations, lasting several minutes. The hallucinations can be visual, auditory, or tactile.
2. What is palinopsia?
Palinopsia is the continuation of visual sensations after cessation of visual stimuli or intermittent reappearance of images (visual perseveration or multiple afterimages). The images are brief and recur periodically in a hemifield. Palinopsia also occurs as a release phenomenon involving lesions of the parietal and occipital lobes, most often in the nondominant hemisphere.
3. What is polyopia?
Polyopia, or cerebral diplopia, is a rare manifestation of occipital cortex lesions. The images are identical in the two eyes, and the number of images seen ranges from one and a half to hundreds. The diplopia of polyopia does not resolve by closing either eye or with pinhole glasses. There is often an associated homonymous hemianopia.
4. What is the Alice in Wonderland syndrome?
The Alice in Wonderland syndrome includes micropsia, macropsia, pelopsia, teleopsia. Size distortion of other sensory modalities may occur. It is often associated with migraines, brain tumors, and the use of psychoactive drugs. It can also be the initial symptom of the Epstein–Barr virus (mononucleosis).
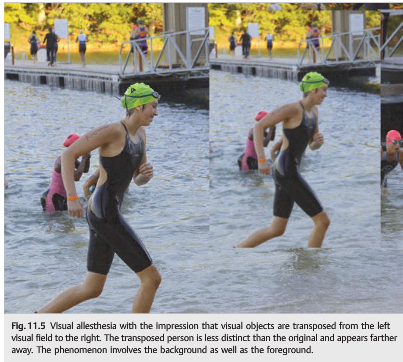
5. What is visual allesthesia?
Visual allesthesia occurs when visual stimuli are transposed from one hemifield to another.
6. What is the Riddoch Phenomenon?
The Riddoch phenomenon involves perception of moving targets in a field otherwise blind to static stimuli. It is seen in occipital lesions.
7. What is Blindsight?
In blindsight, patients who state they are completely blind in one hemifield and are not aware of a visual stimulus in the blind hemifield, nevertheless guess at a level better than chance when asked about some property of the visual stimulus in the hemianopic field.
8. What is Residual Vision?
In residual vision, patients retain some awareness of the target within a dense visual field defect, suggests a severe but relative hemianopia.
9. What 5 conditions are associated oscillopsia?
– 1. Abnormality of the vestibulo-ocular reflex caused by damage of the vestibular system
– 2. Nystagmus
– 3. Tullio phenomenon (noise-induced peripheral vestibular dysfunction)
– 4. Superior oblique myokymia (one eye)
– 5. Pulsating orbital mass (one eye).
10. What is the Anton Syndrome?
In the Anton syndrome, patients with cerebral blindness (bilateral occipital lesions) are not aware of their visual loss and insist that they can see. It is a denial syndrome of unknown mechanism.
Explanation:
“11.3.5 Narcolepsy
Visual hallucinations are a common presenting complaint of narcolepsy. They are described as colorful images, which may involve people, animals, and panoramic scenes.
Patients often have a vague sense that someone else is in the room. They also realize that what they’re experiencing is not a dream and that they are awake.
The classic tetrad of narcolepsy includes the following:
● Cataplexy (transient loss of muscle tone)
● Sleep paralysis (inability to move when the patient first wakes up)
● Sleep attacks (overwhelming sense of fatigue causing the patient to fall asleep for 10 to 30minutes)
● Hypnogogic (entering sleep) and hypnopompic (awakening) hallucinations, lasting several minutes. The hallucinations can be visual, auditory, or tactile.
11.3.6 Palinopsia
Palinopsia is the continuation of visual sensations after cessation of visual stimuli or intermittent reappearance of images (visual perseveration or multiple afterimages) (▶Fig. 11.4). The images are brief and recur periodically in a hemifield. Palinopsia also occurs as a release phenomenon involving lesions of the parietal and occipital lobes, most often in the nondominant hemisphere.
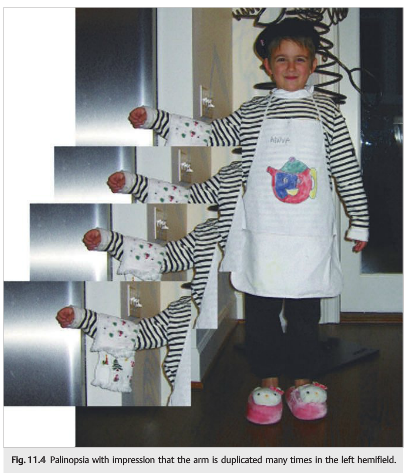
The following are the most common causes of palinopsia:
● Drugs: lysergic acid diethylamide (LSD), neuroleptics
● Migrainous visual aura
● Seizures: temporal, occipital
● Focal cerebral lesions: parietal and occipital lobe lesions, most often in the nondominant hemisphere
● Creutzfeldt–Jakob disease
● Encephalopathies: carbon monoxide poisoning, hepatic encephalopathy, hyperglycemia, and hypoglycemia
11.3.7 Polyopia (Cerebral Diplopia)
Polyopia, or cerebral diplopia, is a rare manifestation of occipital cortex lesions. The Images are identical in the two eyes, and the number of images seen ranges from one and a half to hundreds. The diplopia or polyopia does not resolve by closing either eye and does not improve with pinhole glasses. There is often an associated homonymous hemianopia.
11.3.8 Dysmetropsia (Dysmegalopsia or Metamorphopsia)
Dysmetropsia (also known as dysmegalopsia or metamorphopsia) is a disorder of size perception, where objects can appear smaller (micropsia) or larger (macropsia). Causes Include retinal disorders (most common; one eye only) and migraine (Alice in Wonderland syndrome; both eyes).
11.3.9 Visual Allesthesia
Visual allesthesia occurs when visual stimuli are transposed from one hemifield to another (▶Fig. 11.5). It is usually brief, and most patients experience recurrent episodes. It is seen most often with parieto-occipital lesions or as part of the migrainous visual aura.
The following are the most common causes of palinopsia:
● Drugs: lysergic acid diethylamide (LSD), neuroleptics
● Migrainous visual aura
● Seizures: temporal, occipital
● Focal cerebral lesions: parietal and occipital lobe lesions, most often in the nondominant hemisphere
● Creutzfeldt–Jakob disease
● Encephalopathies: carbon monoxide poisoning, hepatic encephalopathy, hyperglycemia, and hypoglycemia
11.3.7 Polyopia (Cerebral Diplopia)
Polyopia, or cerebral diplopia, is a rare manifestation of occipital cortex lesions. The Images are identical in the two eyes, and the number of images seen ranges from one and a half to hundreds. The diplopia or polyopia does not resolve by closing either eye and does not improve with pinhole glasses. There is often an associated homonymous hemianopia.
11.3.8 Dysmetropsia (Dysmegalopsia or Metamorphopsia)
Dysmetropsia (also known as dysmegalopsia or metamorphopsia) is a disorder of size perception, where objects can appear smaller (micropsia) or larger (macropsia). Causes Include retinal disorders (most common; one eye only) and migraine (Alice in Wonderland syndrome; both eyes).
11.3.9 Visual Allesthesia
Visual allesthesia occurs when visual stimuli are transposed from one hemifield to another (▶Fig. 11.5). It is usually brief, and most patients experience recurrent episodes. It is seen most often with parieto-occipital lesions or as part of the migrainous visual aura.
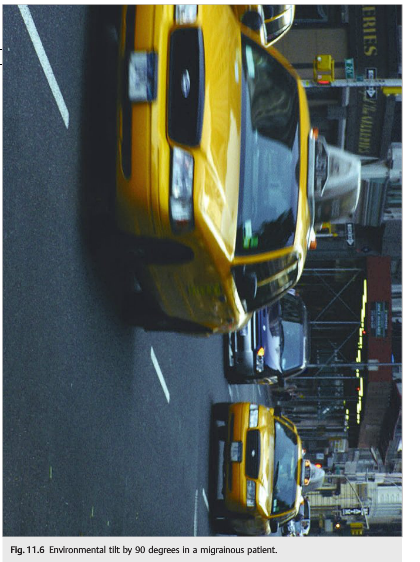
11.3.10 Sensation of Environment Tilt
The sensation of environment tilt phenomenon involves the acute tilt of the environment by 90 or 180 degrees (▶Fig. 11.6). It is brief and spontaneously resolving. The phenomenon is most often associated with the lateral medullary syndrome. It is also described in patients with occipital lesions or migraine with aura.
11.3.11 Riddoch Phenomenon
The Riddoch phenomenon involves perception of moving targets in a field otherwise blind to static stimuli due to an occipital lesion.
11.3.12 Blindsight and Residual Vision
It has been suggested that lesions of the geniculostriate pathway do not eliminate all visual function within the resulting blind region. In blindsight, patients who state they are completely blind in one hemifield and are not aware of a visual stimulus in the blind hemifield, nevertheless guess at a level better than chance when asked about some property of the visual stimulus. In residual vision, patients retain some awareness of the target within a dense visual field defect, suggesting a severe but relative hemianopia.
11.3.13 Oscillopsia
Oscillopsia is the illusion of movement of the environment, often due to any of the following:
● Abnormality of the vestibulo-ocular reflex caused by damage to the vestibular system
● Nystagmus
● Tullio phenomenon (noise-induced peripheral vestibular dysfunction)
● Superior oblique myokymia (one eye)
● Pulsating orbital mass (one eye)
11.3.14 Anton Syndrome
In Anton syndrome, patients with cerebral blindness (bilateral occipital lesions) are not aware of their visual loss and insist that they can see. It is a denial syndrome of unknown mechanism.
11.4 Drugs and Toxins
Numerous drugs and toxins produce visual hallucinations and illusions. The following are some of the most common:
● Postoperative delirium: transient hallucinations after general anesthesia
● Hallucinogens:
○ Cocaine, LSD, marijuana, mescaline, opiates, phencyclidine hydrochloride (PCP),psilocybin and psilocin (hallucinogenic mushroom), and 3,4-methylenedioxy-N-methylamphetamine (MDMA; Ecstasy or Molly).
○ LSD is responsible for delayed impressions of déjà vu or flashbacks that may occur years after even a single LSD use.
● All anticholinergic agents (including atropine, scopolamine, and cyclopentolate)
● All antiparkinsonian agents (dopamine agonists, bromocriptine, anticholinergic agents, etc.)
● Antidepressants
● Antipsychotics
● Digoxin: toxic levels are associated with xanthopsia (illusion of abnormal colors—yellow and green are typical).
● Phosphodiesterase-5 inhibitors (erectile dysfunction medications): bluish vision
● Alcohol
Withdrawal of alcohol and benzodiazepines will also produce hallucinations.
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.