Questions:
1. What is the Balint syndrome and where is its lesion?
2. What is the Gerstmann syndrome and where is its lesion?
3. What is hemineglect and where is its lesion?
4. What are the symptoms of posterior cortical atrophy and where is its lesion?
5. What are the visual symptoms of Alzheimer disease and when in the course of the disease are they likely to occur?
6. What visual symptoms may occur in Creutzfeldt–Jakob disease?
____________________________________________________
Questions with answers:
1. What is the Balint syndrome and where is its lesion?
Balint syndrome is the triad of 1. ocular apraxia, 2. optic ataxia, and 3. simultagnosia. It results most frequently from bilateral parieto-occipital cortical or white matter injury, such as from watershed infarctions, progressive multifocal leukoencephalopathy, Alzheimer disease, and Creutzfeldt–Jakob disease.
2. What is the Gerstmann syndrome and where is its lesion?
Gerstmann syndrome is a combination of right-left confusion, finger agnosia, acalculia, and agraphia. It is caused by lesions in the dominant parietal lobe.
3. What is hemineglect and where is its lesion?
Patients with hemineglect do not notice or respond to stimuli on the side contralateral to the lesion. Hemineglect can affect not only vision but also other sensory and motor modalities. Hemineglect usually occurs from lesions of the nondominant (right) hemisphere. It is associated with damage to various components of a cerebral attentional network, which includes the inferior parietal lobe, the frontal cortex, and the thalamus.
4. What are the symptoms of posterior cortical atrophy and where is its lesion?
Posterior cortical atrophy is characterized by a progressive illness combining memory impairment, insight and judgment impairment, alexia with or without agraphia, visual agnosia, and components of Balint syndrome, Gerstmann syndrome, and transcortical sensory aphasia (fluent aphasia with intact ability to repeat). Neuroimaging reveals cerebral atrophy, more severe posteriorly. Etiologies include Alzheimer disease and other dementias.
5. What are the visual symptoms of Alzheimer disease and when in the course of the disease are they likely to occur?
Alzheimer disease is a slowly progressive degenerative dementia that is often associated with visual disturbances (e.g., difficulty reading), which may predominate early in the course of the disease. Although these patients have numerous visual complaints (e.g., difficulty reading, difficulty seeing, and difficulty processing what they see), they have normal visual acuity and normal ocular examination, and frequently even normal visual fields, and the correct diagnosis is often delayed
6. What visual symptoms may occur in Creutzfeldt–Jakob disease?
The Heidenhain variant of sporadic Creutzfeldt–Jakob Disease manifests with early, prominent visual complaints (e.g., visual hallucinations, difficulty reading, homonymous hemianopia, and distortion of vision).
Explanation: “10.2 Clinical and Radiologic Findings of Specific Disorders
10.2.1 Balint Syndrome
Balint syndrome results most frequently from bilateral parieto-occipital cortical or white matter injury, such as from watershed infarctions, progressive multifocal leukoencephalopathy, Alzheimer disease, and Creutzfeldt–Jakob disease. It associates (1) ocular apraxia (deficit in shifting gaze), (2) optic ataxia (defect in reaching under visual guidance), and (3) simultagnosia (inability to grasp the entire meaning of a picture despite an intact capacity to recognize the picture’s individual constituent elements). Affected patients may be unable to identify a picture of a landscape, but they may be able to identify a small tree within the picture; alternatively, they may be able to read the individual 20/20 letters on the Snellen chart but may not be able to identify a whole word.
10.2.2 Gerstmann Syndrome
Gerstmann syndrome is caused by lesions in the dominant parietal lobe, and therefore, aphasia is often (but not always) present as well, which can make the diagnosis difficult or impossible.
Gerstmann syndrome is a combination of right-left confusion, finger agnosia (loss in the ability to distinguish, name, or recognize the fingers), acalculia (acquired difficulty performing simple mathematical tasks), and agraphia (acquired inability to communicate through writing).
10.2.3 Hemineglect
Hemineglect usually occurs from lesions of the nondominant (right) hemisphere.Patients with hemineglect do not notice or respond to stimuli on the contralateral side.Hemineglect can affect not only vision but also other sensory and motor modalities. It is associated with damage to various components of a cerebral attentional network, which includes the inferior parietal lobe, the frontal cortex, and the thalamus.
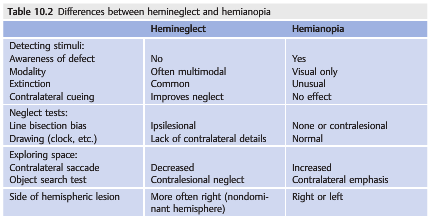
▶Table 10.2 lists the differences between hemineglect and hemianopia, although they can also coexist.
10.3 Causes of Disorders of Higher Cortical Functions
Cerebral disturbances of vision can be caused by any condition that affects the visual association cortices or subcortical white matter. They commonly result from bilateral cerebral lesions and are most often found in patients with cerebral hypoxia resulting in bilateral watershed infarctions or with bilateral infarctions in the territory of the posterior cerebral arteries, diffuse encephalopathy and encephalitis, and degenerative disorders producing dementia.
Computed tomography (CT) and magnetic resonance imaging (MRI) of the brain are sometimes normal or show nonspecific cerebral atrophy in most degenerative dementias. The diagnosis is often difficult and is delayed in patients in whom visual complaints predominate.
10.3.1 Posterior Cortical Atrophy
Posterior cortical atrophy is characterized by a progressive illness combining memory impairment, insight, and judgment impairment, alexia with or without agraphia, visual agnosia, and components of Balint syndrome, Gerstmann syndrome, and transcortical sensory aphasia (fluent aphasia with intact ability to repeat). Neuroimaging reveals cerebral atrophy, more severe posteriorly. Etiologies include Alzheimer disease and other dementias.
10.3.2 Alzheimer Disease
Alzheimer disease is a slowly progressive degenerative dementia that is often associated with visual disturbances (e.g., difficulty reading), which may predominate early in the course of the disease. Although these patients have numerous visual complaints (e.g., difficulty reading, difficulty seeing, and difficulty processing what they see), they have normal visual acuity and normal ocular examination, and frequently even normal visual fields, and the correct diagnosis is often delayed. Brain CT and MRI are often normal or show some posterior cerebral atrophy at the parieto-occipital junction. Functional imaging, such as positron emission tomography (PET) and single-photon emission computed tomography (SPECT), may help make the diagnosis.
10.3.3 Creutzfeldt–Jakob Disease
Creutzfeldt–Jakob disease is a rapidly progressive dementia that is usually lethal within a few months. Along with kuru, Gerstmann–Sträussler syndrome, and fatal familial insomnia, it comprises a group of dementing illnesses known as human transmissible spongiform encephalopathies. The Heidenhain variant of sporadic Creutzfeldt–Jakob Disease manifests with early, prominent visual complaints (e.g., visual hallucinations, difficulty reading, homonymous hemianopia, and distortion of vision).
The diagnosis is based on the following:
● Normal conventional brain MRI with abnormal diffusion-weighted images
● Abnormal electroencephalogram (periodic activity)
● Positive testing for mutation 14–3–3 in the prion protein gene in the cerebrospinal fluid
● Abnormal brain biopsy”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections totcooper@stanford.edu.