Neuro-ophthalmology Question of the Week: Hallucinations and Illusions 1
Questions:
1. What is the difference between a hallucination and an illusion?
2. Are isolated visual hallucinations common in psychiatric disorders?
3. What is the Pulfrich effect?
4. What is the Charles Bonnet syndrome?
5. Which dementias may be associated with paranoid hallucinations and illusions?
6. What is the duration of migraine with visual aura episodes?
7. What is the duration of visual phenomenon of occipital seizures?
8. What is peduncular hallucinosis and where is its lesion?
____________________________________________________
Questions with answers:
1. What is the difference between a hallucination and an illusion?
Hallucination refers to the perception of a stimulus when in reality, none is present. An Illusion refers to misperception of a stimulus that is present in the external environment.
2. Are isolated visual hallucinations common in psychiatric disorders?
No, many psychiatric illnesses have visual illusions and hallucinations, which are usually associated with other perceptive abnormalities (usually auditory).
3. What is the Pulfrich effect?
The Pulfrich effect (named after Carl Pulfrich) is a well described visual stereo illusion observed when a swinging pendulum bob is viewed through a neutral density filter in front of one eye. The Pulfrich phenomenon is seen in patients with clinical signs of asymmetric optic neuropathy.
4. What is the Charles Bonnet syndrome?
The Charles Bonnet syndrome is characterized by visual hallucinations associated with poor vision in each eye, such as that in advanced macular degeneration. Simple and complex visual hallucinations are present in up to 10% of patients with severe binocular visual loss, presumably because the normal visual cortex has been “released” from anterior visual pathway input. This syndrome is more common in the elderly.
5. Which dementias may be associated with paranoid hallucinations and illusions?
Alzheimer disease, Pick disease, human immunodeficiency virus (HIV) dementia, Huntington’s chorea, Creutzfeldt-Jakob disease, and multi-infarct dementia, may be associated with paranoid hallucinations and illusions.
6. What is the duration of migraine with visual aura episodes?
10-30 minutes
7. What is the duration of visual phenomenon of occipital seizures?
A few seconds.
8. What is peduncular hallucinosis and where is its lesion?
It is a rare neurologic syndrome characterized by vivid, usually formed, colorful hallucinations of people, animals, and complex scenes with motion. It is most often related to a midbrain infarction in the region of the peduncle. Patients usually have sleep/wake disorders and are aware that these images are not real. The hallucination usually begins a few days after the lesion occurs and may persist for weeks to months.
Explanation: “11 Abnormal Visual Perceptions: Hallucinations and Illusions
Abnormal visual perceptions are common in psychiatric disorders, ophthalmic disorders, and neurologic diseases, and can be due to numerous drugs and toxins.
In this chapter, the term hallucination refers to perception of a stimulus when, in reality, none is present, for example, when a patient with delirium tremens describes seeing bugs and snakes on the bedroom walls. The term illusion refers to misperception of a stimulus that is present in the external environment, for example, when an elderly individual interprets a chair in a poorly lit room as a person.
11.1 Psychiatric Disorders
Hallucinations are common in psychotic syndromes. They are most often complex and auditory. Isolated visual hallucinations are uncommon in psychiatric disorders.
Pearls
Primary psychiatric illnesses often cause visual illusions and hallucinations, which are usually associated with other perceptive abnormalities (usually auditory); they are not associated with altered mental status or focal neurologic signs.
11.2 Ophthalmic Disorders
11.2.1 Optical Causes
Optical causes of abnormal visual perceptions include alterations in the tear film (dry eyes and abnormalities in blinking), and irregularities in the cornea (keratoconus and corneal scarring) or the lens (cataract). Entoptic phenomena are visual experiences caused by ocular structures (e.g., floaters).
11.2.2 Retinal Disorders (Maculopathies)
Retinal disorders or maculopathies can produce visual hallucinations.
Metamorphopsias from macular disorders are best detected by the Amsler grid test. Macular edema produces micropsia (increased separation of retinal photoreceptors), and epiretinal membrane produces macropsia (when the photoreceptors are pushed together).
Vitreoretinal traction is responsible for phosphenes (flashing lights). These are more apparent in a dark environment. Floaters (posterior vitreous detachment and vitreous debris) are most noticeable against a uniformly illuminated background. Outer retinal diseases, such as cancer-associated retinopathy, acute zonal occult outer retinopathy, and the multiple evanescent white dot syndrome, may cause simple white flashing lights.
11.2.3 Optic Nerve Disease
Phosphenes are sometimes reported by patients with optic neuropathies. They are sometimes triggered by noise or moving the eye.
Pulfrich phenomenon, or the perception of an elliptical movement when observing a pendulum swinging in one plane, occurs in patients with unilateral or asymmetric optic neuropathies. It is a stereo illusion related to the difference in conduction delay between the two eyes.
11.2.4 Charles Bonnet Syndrome
Charles Bonnet syndrome is characterized by visual hallucinations associated with poor vision, such as in macular degeneration. Simple and complex visual hallucinations are present in up to 10% of patients with severe binocular visual loss, presumably because the normal visual cortex has been “released” from anterior visual pathway input. This Syndrome is more common in the elderly. The hallucinations are not stereotyped and involve vivid scenes of animals, flowers, and people. They may be episodic or continuous and are more common in the evening and when patients have their eyes open. Once patients are reassured, they often tolerate these hallucinations well, but treatment is usually unsuccessful.
11.3 Neurologic Disorders
A variety of encephalopathies or focal cerebral lesions can cause hallucinations and illusions. These symptoms are most often visual and tactile, whereas psychiatric hallucinations are most often auditory. They occur in awake or drowsy patients, who often are not aware that these are hallucinations and may become frightened.
11.3.1 Confusion and Dementia
Confusion and dementia can cause visual hallucinations and illusions.
Delirium tremens is associated with very frightening, well-formed visual hallucinations, including bugs, monsters, and snakes.
Lewy body dementia is commonly associated with visual hallucinations.
Other dementias, such as Alzheimer disease, Pick disease, human immunodeficiency virus (HIV) dementia, Huntington chorea, Creutzfeldt–Jakob disease, and multi-infarct dementia, may be associated with paranoid hallucinations and illusions. Drugs used to treat Parkinson disease can also cause hallucinations.
11.3.2 Migraine
Numerous visual phenomena occur during the visual aura of migraine (▶Table 11.1).These visual phenomena are often positive and therefore can be described as hallucinations.
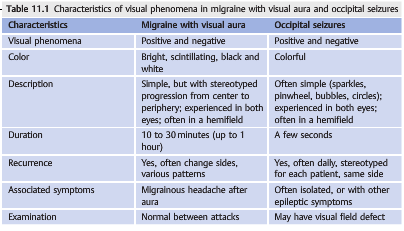
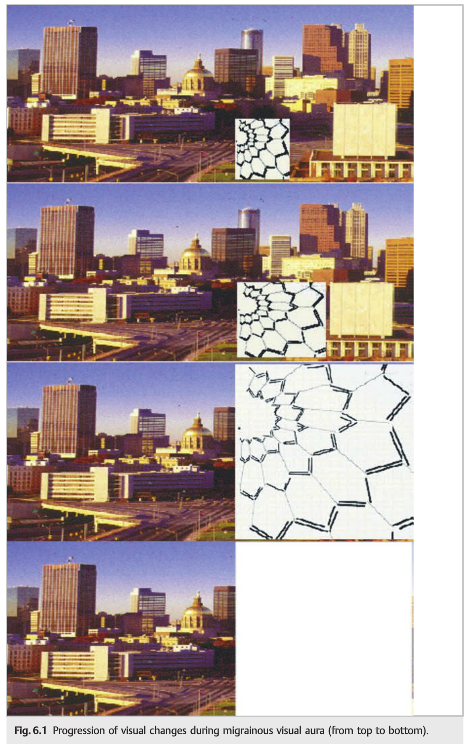
Migrainous visual phenomena usually last between 10 and 30 minutes and progress over time (migrainous march) (see Chapter 6, ▶Fig. 6.1). They may be associated with other neurologic symptoms, such as ipsilateral tingling and speech impairment, and are classically followed by migrainous headaches. Migraineurs are aware that the images they see are not real.
Positive or negative visual phenomena are present in both eyes, either in the entire eye or in one hemifield. Phenomena include phosphenes, which are usually bright or white, and scintillating scotoma, described as progressively enlarging bright scotoma with sharp edges. Distortion of images with micropsia and macropsia (Alice in Wonderland syndrome) or tilting of objects can also occur.
11.3.3 Occipital Seizures
Occipital seizures can cause simple and colorful, positive or negative visual phenomena present in both eyes, including sparkles, pinwheels, bubbles, scotoma, and dots. Although they are often moving, they do not have the stereotyped progression observed in migraine. They are short in duration (usually lasting only a few seconds) and may be isolated. They are usually stereotyped for each patient.
Occipital seizures can occur with a variety of occipital lesions or as part of primary occipital seizures, which are more common in children.
11.3.4 Peduncular Hallucinosis
Peduncular hallucinosis is a rare neurologic syndrome characterized by vivid, usually well-formed, colorful hallucinations of people, animals, and complex scenes with motion. It is most often related to a midbrain infarction in the region of the peduncle, and is also likely a “release phenomenon” (▶Fig. 11.3).
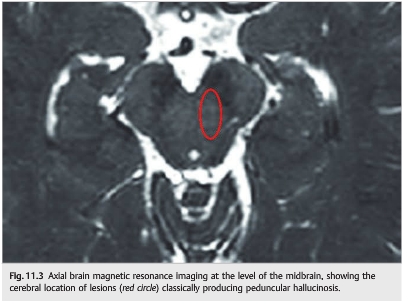
Patients usually have sleep/wake disorders and are aware that these images are not real. The hallucination usually begins a few days after the lesion occurs and may persist for weeks to months.”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections totcooper@stanford.edu.