Questions:
1. What visual symptoms may patients with papilledema report?
2. When is central visual acuity loss experienced in papilledema, early or late?
3. What type of visual field defect is found initially with papilledema?
4. What type of visual field loss is experienced in long-standing papilledema?
5. Can visual loss from papilledema happen with any cause of papilledema?
 1
1
______________________________________________________
Questions with answers:
1. What visual symptoms may patients with papilledema report?
They may complain of “flashing lights” or transient visual obscurations (brief episodes of visual loss occurring in one or both eyes), often precipitated by changes in posture, such as standing up after bending over.
2. When is central visual acuity loss experienced in papilledema, early or late?
In untreated chronic papilledema, central visual acuity is normal until late.
3. What type of visual field defect is found initially with papilledema?
Blind spot enlargement and nasal defects are common initially.
4. What type of visual field loss is experienced in long-standing papilledema?
Patients develop insidious progressive visual field constriction.
5. Can visual loss from papilledema happen with any cause of papilledema?
Visual loss from papilledema happens with any cause of papilledema. Hence it is very important to look for papilledema in all patients with headache or known hydrocephalus, brain tumor, or meningitis and to provide urgent treatment to prevent visual loss when papilledema is present.
Explanation:
“9.5 Classification and Progression of Papilledema
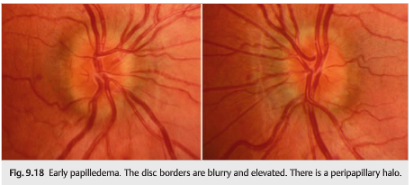
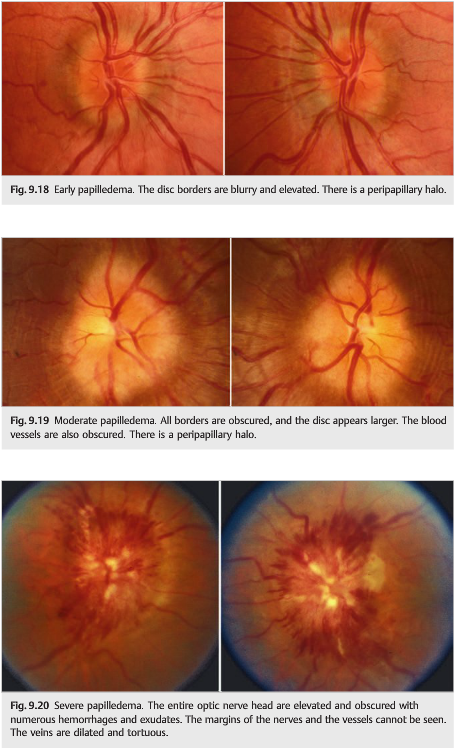
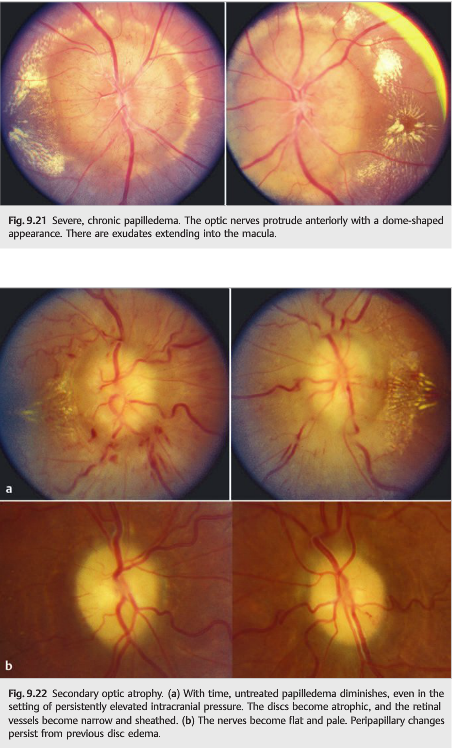
Patients with papilledema often have no visual symptoms initially. They may complain of “flashing lights” or transient visual obscurations (brief episodes of visual loss occurring in one or both eyes), often precipitated by changes in posture, such as standing up after bending over. Untreated chronic papilledema results in visual loss: central visual acuity is normal until late, and patients develop insidious progressive visual field constriction (▶Fig. 9.18, Fig. 9.19, ▶Fig. 9.20, ▶Fig. 9.21, ▶Fig. 9.22).
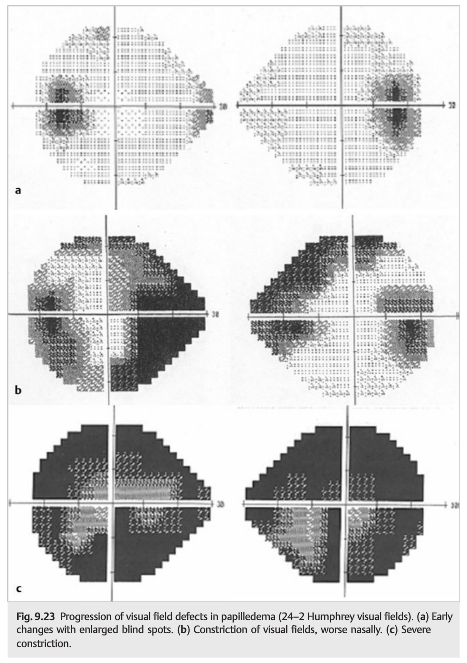
Formal visual field testing (Humphrey perimetry shown in ▶Fig. 9.23) is often abnormal in papilledema. Blind spot enlargement and nasal defects are common initially(top, Fig. 9.23). They may progress, usually circumferentially, to involve the central 30 degrees of the visual field (middle). Severe devastating visual field loss (bottom) is often permanent if raised intracranial pressure is not promptly treated (note that even with the severe visual field loss seen in the bottom example, visual acuity was still relatively preserved at 20/25 OD [right eye] and 20/40 OS [left eye]).
Pearls
Visual loss from papilledema happens with any cause of papilledema. Hence it is very important to look for papilledema in all patients with headache or known hydrocephalus, brain tumor, or meningitis and to prevent visual loss when papilledema is present.
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections totcooper@stanford.edu.