Questions:
1. Once optic disc edema is confirmed, what should be determined?
2. In anterior optic neuropathy with disc edema is visual acuity usually decreased?
3. In papilledema is visual acuity usually decreased?
4. In anterior optic neuropathy with disc edema is color vision usually decreased?
5. In papilledema is color vision usually decreased?
6. What are the usual characteristics of visual field defects in anterior optic neuropathy with disc edema?
7. What are the usual characteristics of visual field defects in papilledema?
8. Is anterior optic neuropathy with disc edema usually unilateral?
9. Is papilledema usually unilateral?
10. What findings are often associated with papilledema?
11. Does the absence of disc edema rule out raised intracranial pressure in a patient presenting with headache?
12. Does the absence of spontaneous retinal venous pulsations at the disc rule-out elevated intracranial pressure?
 1
1
____________________________________________________
Questions with answers:
1. Once optic disc edema is confirmed, what should be determined?
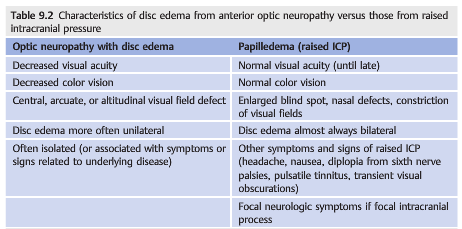
Once optic disc edema is confirmed, it should be determined whether it is related to an optic nerve disorder (optic neuropathy) or to raised intracranial pressure (papilledema).
2. In anterior optic neuropathy with disc edema is visual acuity usually decreased?
Yes
3. In papilledema is visual acuity usually decreased?
No
4. In anterior optic neuropathy with disc edema is color vision usually decreased?
Yes
5. In papilledema is color vision usually decreased?
No
6. What are the usual characteristics of visual field defects in anterior optic neuropathy with disc edema?
Central, arcuate, and altitudinal defects
7. What are the usual characteristics of visual field defects in papilledema?
Enlarged blind spots, nasal defects, and generally constricted
8. Is anterior optic neuropathy with disc edema usually unilateral?
Yes
9. Is papilledema usually unilateral?
No
10. What findings are often associated with papilledema?
Symptoms of increased ICP (headache, nausea, diplopia from 6th nerve palsies, pulsatile tinnitus and transient visual obscurations) and focal neurologic signs or symptoms may be present if there is a focal intracranial process.
11. Does the absence of disc edema rule out raised intracranial pressure in a patient presenting with headache?
Although papilledema is a reliable sign of raised intracranial pressure, the absence of disc edema does not rule out raised intracranial pressure in a patient presenting with headache.
12. Does the absence of spontaneous retinal venous pulsations at the disc rule-out elevated intracranial pressure?
No.
Explanation: “9.4 Evaluation of the Patient with Disc Edema
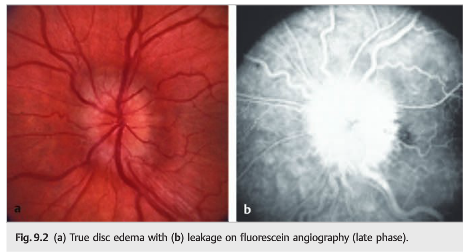
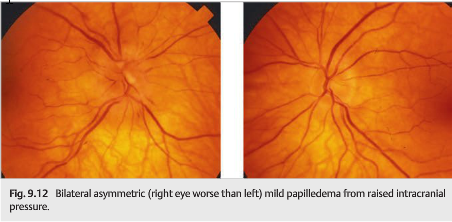
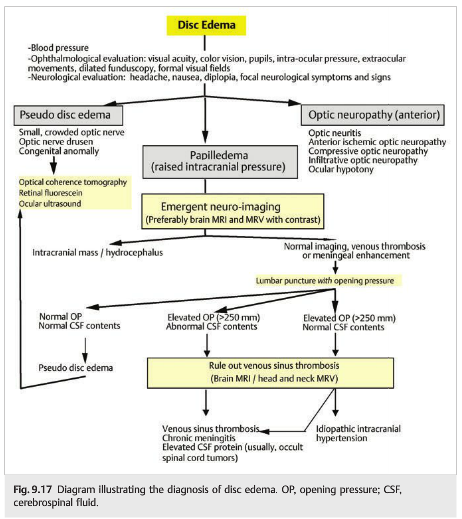
Once optic disc edema is confirmed, it should be determined whether it is related to an optic nerve disorder (optic neuropathy) or to raised intracranial pressure. Papilledema Is the term used to describe optic disc edema resulting from raised intracranial pressure (▶Fig. 9.12). All other optic disc edema is termed disc edema or swollen optic nerve. ▶Table 9.2 compares the characteristics of disc edema from anterior optic neuropathy with those from raised intracranial pressure.
Most disorders producing raised intracranial pressure are life-threatening emergencies. The finding of papilledema should prompt an immediate workup, ideally in a specialized center with up-to-date neuroimaging, as well as neurologic and ophthalmological consultations.
The workup should include the following:
● Looking for an underlying neurologic process
● Careful evaluation of the visual function (visual acuity and formal visual field testing),as papilledema can result in permanent visual loss from secondary optic atrophy
● Checking blood pressure (severe systemic hypertension or malignant hypertension may produce bilateral disc edema that mimics papilledema)
Pearls
Although papilledema is a reliable sign of raised intracranial pressure, the absence of disc edema does not rule out raised intracrani intracranial pressure in a patient presenting with headache.
The mechanisms responsible for raised intracranial pressure and papilledema are as follows:
● Hydrocephalus
● Intracranial mass
○ Tumor, abscess
○ Intracerebral hemorrhage○ Subdural/epidural hemorrhage○ Large vascular malformation
● Meningeal process○ Infectious
○ Inflammatory
○ Neoplastic
● Increased venous pressure
● Cerebral venous thrombosis
● Idiopathic intracranial hypertension
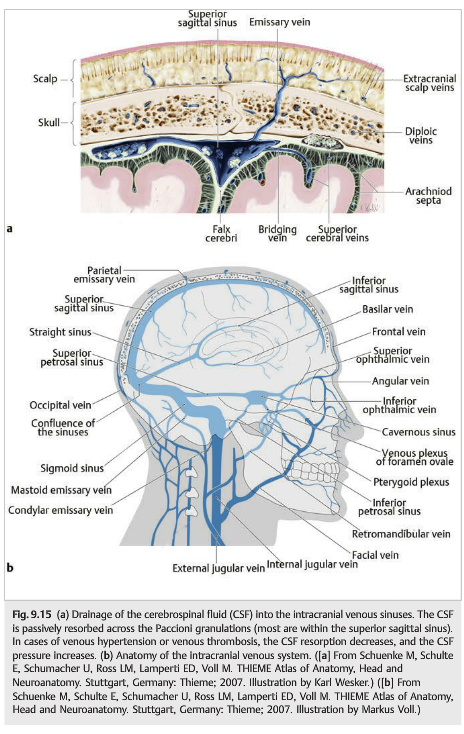
Increased venous pressure produces symptoms and signs of raised intracranial pressure, including papilledema.
The causes of increased venous pressure include all of the causes of decreased venous return (▶Fig. 9.15):
● Right cardiac insufficiency
● Pulmonary hypertension
● Sleep apnea syndrome
● Superior vena cava syndrome
● Jugular vein occlusion
● Dural fistula
● Cerebral venous stenosis
● Cerebral venous thrombosis
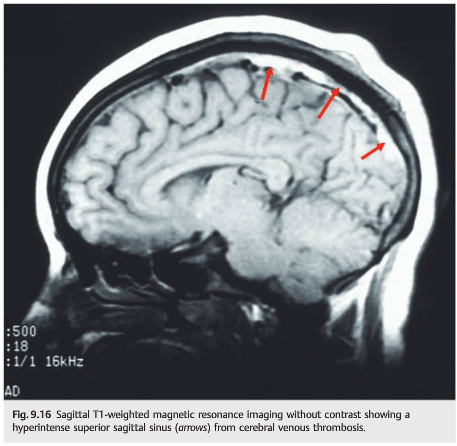
Cerebral venous thrombosis is a classic cause of raised intracranial pressure (▶Fig. 9.16; see also Chapter 20). Patients may present with isolated raised intracranial pressure, thereby mimicking idiopathic intracranial hypertension. Early recognition may prevent a devastating stroke and visual loss from chronic papilledema.
When evaluating a patient with presumed papilledema (raised intracranial pressure), neuroimaging needs to be obtained emergently to rule out an intracranial process (▶Fig. 9.17). Magnetic resonance imaging (MRI) with contrast of the brain is the ideal test and is the most sensitive to detect intracranial masses, infiltrative and meningeal processes, and cerebral venous thrombosis. Computed tomography (CT)without contrast, which is often the test of choice in the emergency room, is in most cases not helpful in these patients, unless it is followed by brain MRI. Indeed, the CT is helpful to detect intracranial hemorrhages, hydrocephalus, and large mass lesions, but it does not rule out any of the other intracranial lesions. Patients with a normal head CT should be investigated further with brain MRI (see Chapter 4). A normal brain MRI scan in the setting of papilledema suggests a meningeal process, venous hypertension, or idiopathic intracranial hypertension as the cause of raised intracranial pressure. A Lumbar puncture with measurement of the cerebrospinal fluid (CSF) opening pressure and CSF analysis should always be performed.
Spontaneous Retinal Venous Pulsations
Background: The validity of the clinical dictum
“the presence of spontaneous retinal venous pulsation (SVP) excludes raised intracranial pressure” has not been previously tested. We set out to determine the specificity and positive predictive value (PPV) of the presence of SVP to indicate normal intracranial pressure (ICP) in a routine clinical setting.
Methods: We prospectively recruited patients undergoing lumbar puncture (LP), and 2 clinicians were blinded to the indications for LP and cerebrospinal fluid opening pressure (OP). Interobserver reliability was assessed.
Results: There were 106 patients in our cohort with a median age of 44 years (range, 18-79 years) and median body mass index of 27.5 kg/m (range, 18-48 kg/m). SVP was present in 94 of 106 patients (88.7%). Thirteen of 106 (12.3%) patients had high OP (≥30 cmH2O), and SVP was present in 11 of 13 patients (86%) with high OP. The sensitivity (95% confidence interval) of the presence of SVP to exclude raised ICP was 0.89 (0.88-0.92), specificity of 0.15 (0.05-0.37), PPV of 0.88 (0.87-0.9), and negative predictive value of 0.17 (0.05-0.4). Interobserver agreement was moderate for SVP (kappa = 0.42).
Conclusions: Although the sensitivity and PPV of the presence of SVP to exclude raised ICP is high, it is not absolute. SVP can be seen in some patients with high ICP. Relying on the presence of SVP to exclude raised ICP may give a false sense of reassurance.2
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
2. The Clinical Validity of the Spontaneous Retinal Venous Pulsation. Wong and White: J Neuro-Ophthalmol 2013 Mar;33(1):17-20.
References:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
2. The Clinical Validity of the Spontaneous Retinal Venous Pulsation. Wong and White: J Neuro-Ophthalmol 2012.
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.