Questions:
1. What should be checked on all head trauma patients?
2. What are the mechanisms of traumatic optic neuropathy?
3. What imaging should be ordered when traumatic optic neuropathy is suspected?
4. What treatment is usually required for direct traumatic optic neuropathies?
5. What treatment is usually required for indirect traumatic optic neuropathies?
 1
1
____________________________________________________
Questions with answers:
1. What should be checked on all head trauma patients?
All head trauma patients should have their the visual acuity measured and the pupils checked for the presence of a RAPD.
2. What are the mechanisms of traumatic optic neuropathy?
The optic nerve may be injured directly by an orbital foreign body or by a bone fragment in case of orbital fracture (direct traumatic optic neuropathy); or indirectly, as a result of concussive forces to the head, particularly the forehead (indirect traumatic optic neuropathy).
3. What imaging should be ordered when traumatic optic neuropathy is suspected?
Obtain a CT scan of the brain and orbits without contrast and with bone windows.
4. What treatment is usually required for direct traumatic optic neuropathies?
Direct traumatic optic neuropathies usually require emergent surgical treatment to decompress the optic nerve and treat the fracture.
5. What treatment is usually required for indirect traumatic optic neuropathies?
The management of indirect traumatic optic neuropathy is controversial. Although visual loss may be devastating and permanent, vision may also recover spontaneously. There is no indication for surgical decompression of the injured optic nerve, and corticosteroids especially in very high doses are not helpful and may even be harmful when administered more than 8 hours after injury. In addition, the use of corticosteroids should be avoided in patients with systemic traumatic injuries and traumatic brain injury.
Explanation: “8.9 Traumatic Optic Neuropathy
Traumatic optic neuropathy is an uncommon but potentially devastating complication of head injury. It should always be suspected in any patient with evidence of optic nerve dysfunction (e.g., otherwise unexplained decreased visual acuity, RAPD, or dyschromatopsia) following head trauma. Because of associated neurologic deficits and other traumatic injuries, the diagnosis is often delayed. However, systematic examination of the pupils in the emergency room (looking for a RAPD) should allow early diagnosis, even in unresponsive patients
8.9.1 Mechanism
The optic nerve may be injured directly by an orbital foreign body or by a bone fragment in case of orbital fracture (direct traumatic optic neuropathy; ▶Fig. 8.41), or indirectly, as a result of concussive forces to the head, particularly the forehead (indirect traumatic optic neuropathy; (▶Fig. 8.42). The latter causes both a mechanical and ischemic insult to the optic nerve, likely at the level of the optic canal.

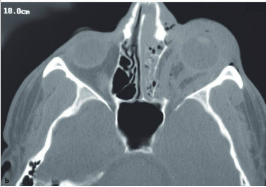
Fig.8.41 Direct traumatic left optic neuropathy. (a) Left orbital trauma with enophthalmos, impaired motility in the left eye, and profound left visual loss. There is a left relative afferent pupillary defect, and the fundus is normal. (b) Computed tomographic scan of the brain and orbits without contrast (bone window) showing an extensive fracture of the left medial wall of the orbit, involving the optic canal.
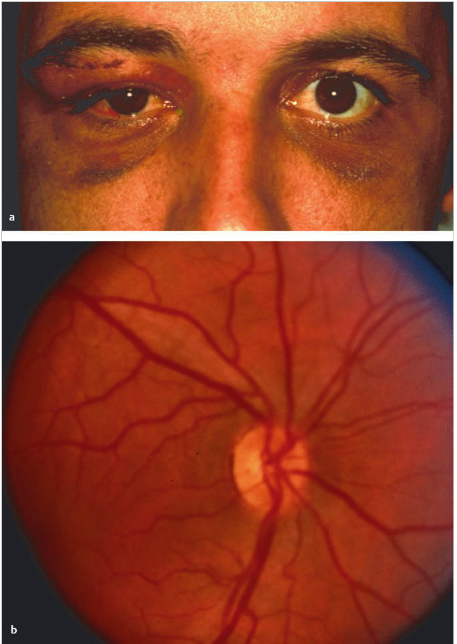
Fig.8.42 Indirect traumatic right optic neuropathy. (a) Facial trauma with bilateral periorbital ecchymosis and indirect traumatic optic neuropathy. There is visual loss in the right eye, and pupil examination shows a right relative afferent pupillary defect. The fundus is normal. The computed tomographic scan of the brain and orbits is normal. There is no fracture and no orbital foreign body. (b) Mild optic nerve pallor 6 weeks later.
8.9.2 Treatment
Direct traumatic optic neuropathies usually require emergent surgical treatment to decompress the optic nerve and treat the fracture.
The management of indirect traumatic optic neuropathy is controversial. Although Visual loss may be devastating and permanent, vision may also recover spontaneously. There is no indication for surgical decompression of the injured optic nerve, and corticosteroids (even very high doses) are not helpful and may even be harmful when administered more than 8 hours after injury. In addition, the use of corticosteroids should be avoided in patients with systemic traumatic injuries and traumatic brain injury who are at risk for infectious complications.
Pearls
Check the visual acuity and the pupils of all trauma patients. If abnormal, request an ophthalmology consultation. Obtain a CT scan of the brain and orbits without contrast and with bone windows.”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.