Questions:
1. How frequently are drusen present in the general population?
2. What techniques may be useful to demonstrate buried disc drusen?
3. What should be done with symptomatic patients with optic disc drusen?
4. What test should be done in all patients with optic nerve hypoplasia?
5. When is a visual field defect expected to be seen with intraocular myelination?
6. What visual field defect would be most likely with intraocular myelination?
7. What test should be done in patients with optic disc coloboma or the “morning glory” disc anomaly?
8. What visual field defect may be associated with tilted discs?
9. What findings are likely with an optic disc pit?
 1
1
____________________________________________________
Questions with answers:
1. How frequently are drusen present in the general population?
Drusen are small, calcific concretions present in the optic nerve of 1 to 2% of the population.
2. What techniques may be useful to demonstrate buried disc drusen?
Buried drusen can be seen with autofluorescence imaging of the optic nerves, OCT, B-scan ultrasonography and CT scan of the orbits.
3. What should be done with symptomatic patients with optic disc drusen?
Symptomatic patients should undergo an evaluation for other causes of optic neuropathies because, in some cases, the optic nerve drusen are a red herring.
4. What test should be done in all patients with optic nerve hypoplasia?
A brain MRI scan looking for septo-optic dysplasia and pituitary ectopia should be obtained in all cases of optic nerve hypoplasia. All patients with septo-optic dysplasia or pituitary ectopia also need an endocrine evaluation looking for panhypopituitarism, which may be life threatening when not diagnosed.
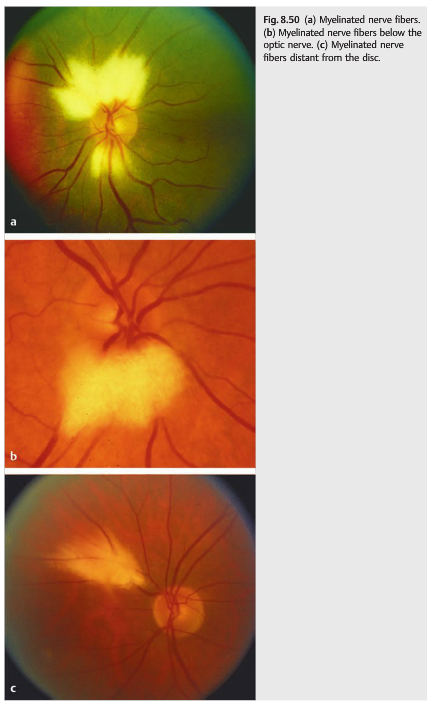
5. When is a visual field defect expected to be seen with intraocular myelination?
Visual field defects are seen only with extensive intraocular myelination.
6. What visual field defect would be most likely with intraocular myelination?
Usually the VF defect will be an enlarged blind spot when the myelination surrounds the optic disc.
7. What test should be done in patients with optic disc coloboma or the “morning glory” disc anomaly?
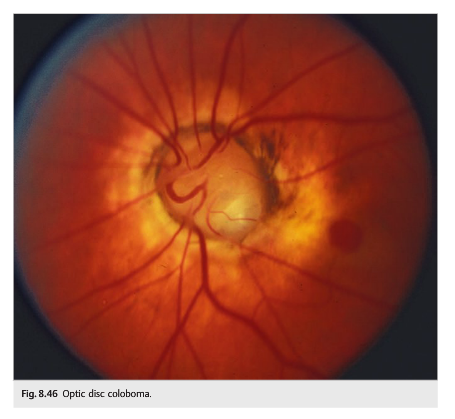
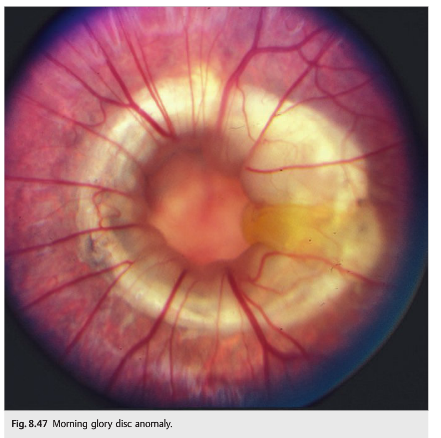
Optic disc colobomas are isolated or can be associated with coloboma of the iris, retina, and choroid. It may rarely be associated with forebrain abnormalities (basal encephalocele) and warrants routine neuroimaging. The “morning glory” disc anomaly is associated with transsphenoidal basal encephaloceles and also warrants routine neuroimaging.
8. What visual field defect may be associated with tilted discs?
Tilted disc anomaly arises when the optic nerve enters the sclera at an oblique angle. It is common in high myopes and often results in relative bitemporal visual field defects that do not respect the vertical meridian.
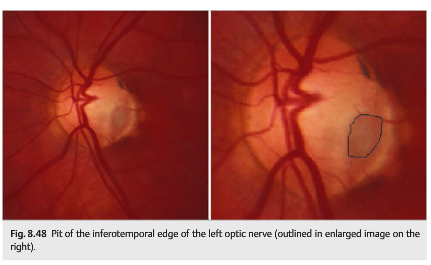
9. What findings are likely with an optic disc pit?
It is characterized by a small excavation of the neuroretinal rim of the optic disc and usually involves the inferotemporal portion of the optic nerve. The missing area is often associated with an arcuate visual field defect. Optic pit may also be associated with serous detachment of the macula, causing decreased visual acuity.
Explanation: “8.11 Optic Nerve Anomalies
8.11.1 Optic Nerve Head Drusen
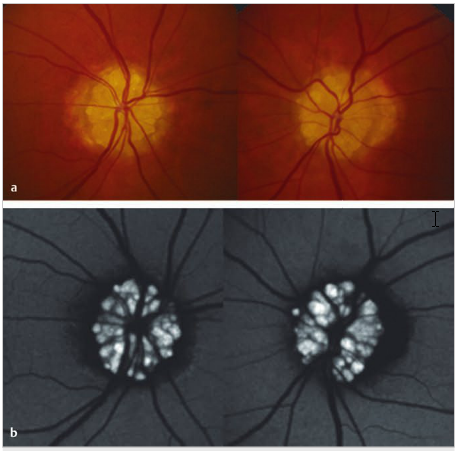
Drusen are small, calcific concretions present in the optic nerve of 1 to 2% of the population (▶Fig. 8.44). Autosomal dominant transmission is suspected in most cases. Optic nerve head drusen are usually bilateral, but they may be asymmetric. They may be visible on fundus examination in teenagers and in adults (often buried in younger children) and may slowly increase over time. They are often asymptomatic and discovered during routine fundus examination. Some patients have brief episodes of transient visual obscurations. The drusen may mimic disc edema when they are buried in the optic nerve head. They may result in peripheral visual field defects, which may worsen slowly over time (optic nerve head drusen usually do not produce central visual loss). The diagnosis is easy when the drusen are superficial and seen on funduscopic examination. Buried drusen can be seen with autofluorescence imaging of the optic nerves, OCT, B-scan ultrasonography and CT scan of the orbits showing calcifications in the optic nerve heads (▶Fig. 8.44).
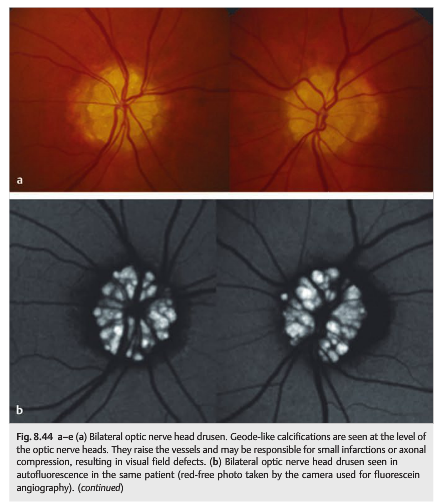
Pearls
Incidentally found optic nerve drusen are common and are usually asymptomatic. Symptomatic patients should undergo an evaluation for other causes of optic neuropathies because, in some cases, the optic nerve drusen are a red herring.
8.11.2 Congenital Disc Anomalies
Congenital disc anomalies may be isolated or associated with systemic disorders or malformations. The level of visual loss associated with congenital disc anomalies varies from minimal visual dysfunction to total blindness. In childhood, the most common presentation of unilateral disc anomaly is strabismus, whereas those with bilateral disc anomalies more frequently present with poor vision or nystagmus. Some may also be diagnosed during adulthood on a routine funduscopic examination.
Optic Nerve Hypoplasia
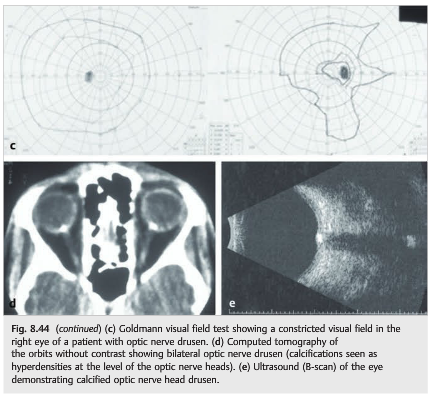
Optic nerve hypoplasia (▶Fig. 8.45) is the most common congenital optic nerve anomaly. It is characterized by a small optic nerve (reduced diameter), sometimes with peripapillary halo (double ring sign), and may be unilateral or bilateral.
Pearl
A brain MRI scan looking for septo-optic dysplasia and pituitary ectopia should be obtained in all cases of optic nerve hypoplasia. All patients with septo-optic dysplasia or pituitary ectopia need an endocrine evaluation looking for panhypopituitarism, which may be life threatening when not diagnosed.
Classic systemic and teratogenic associations with optic nerve hypoplasia include the following:
● Midline developmental abnormalities
○ Septo-optic dysplasia (de Morsier syndrome): absent septum pellucidum, thin corpus callosum, hypopituitarism with pituitary ectopia
● Albinism, aniridia, Duane syndrome, and numerous other congenital ocular syndromes
● Maternal diabetes
● Fetal alcohol syndrome
● Drugs or substances taken by the mother during pregnancy, such as phenytoin, quinine, phencyclidine hydrochloride (PCP), lysergic acid diethylamide (LSD), and alcohol
Optic Disc Coloboma
Optic disc coloboma is faulty closure of the embryonic fetal fissure of the optic stalk and cup. It is isolated or associated with coloboma of the iris, retina, and choroid. A rare association with forebrain abnormalities (basal encephalocele) warrants routine neuroimaging of patients with colobomas. Characteristic features of the optic disc coloboma(▶Fig. 8.46) include excavation within the optic disc, asymmetric defect, vision varying based on size and location of the coloboma within the disc, and minimal peripapillary pigmentary changes. Retinal vasculature is normal.
Morning Glory Disc Anomaly
The mechanism behind “morning glory” disc anomaly is debated, but it results at least partially from faulty closure of the embryonic fetal fissure of the optic stalk and cup. Its association with transsphenoidal basal encephaloceles warrants routine neuroimaging of patients with such anomalies. Characteristic features of morning glory disc anomaly (▶Fig. 8.47) include congenital funnel-shaped excavation of the posterior pole of the fundus (the optic disc lies within the excavation), severe peripapillary pigmentary changes, and anomalous straightening of the retinal vasculature.
Optic Pit
Optic pit (▶Fig. 8.48) results from faulty closure of the embryonic fetal fissure of the optic stalk and cup (same as coloboma, which is a more severe variant). It is characterized by a small excavation of the neuroretinal rim of the optic disc and usually involves the inferotemporal portion of the optic nerve. The missing area is often associated with an arcuate visual field defect. Optic pit may be associated with serous detachment of the macula, causing decreased visual acuity.
Tilted Disc Anomaly
Tilted disc anomaly (▶Fig. 8.49) arises when the optic nerve enters the sclera at an oblique angle. It is common in high myopes and often results in relative bitemporal visual field defects that do not respect the vertical meridian.

Myelinated Nerve Fibers
The optic nerve fibers behind the lamina cribrosa are normally myelinated. Usually, myelin does not enter the eye. Intraocular myelination of retinal nerve fibers is seen in <1% of the population (▶Fig. 8.50). Visual field defects are seen only with extensive intraocular myelination, usually in the form of an enlarged blind spot when the myelination surrounds the optic disc.
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
These questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.