Questions:
1. What historical factors are important to assess in a patient with suspected optic neuropathy?
2. What tests should be considered based on the assessment of appropriate historical factors?
 1
1
____________________________________________________
Questions with answers:
Question 1. What historical factors are important to assess in a patient with suspected optic neuropathy?
A. Cat exposure
B. Recent travel
C. Tick bite
D. Immunosuppression
E. Associated systemic symptoms and sign
F. Associated neurologic symptoms and signs, including focal neurologic signs; a history of vertigo, diplopia, numbness, Lhermitte sign, or Uhthoff Phenomenon; headaches; and meningismus
G. Associated ocular findings, including intraocular inflammation and retinitis.
Question 2. What tests should be considered based on the assessment of appropriate historical factors?
A. MRI of the brain and orbits with contrast (confirms optic nerve enhancement and looks for demyelinating disease in the brain)
B. Chest radiograph (looking for sarcoidosis)
C. Blood tests (vary based on presumed diagnosis): CBC, platelets, angiotensin-converting enzyme (ACE) level, and syphilis testing
D. Lumbar puncture: performed when an infectious cause or underlying systemic inflammatory disease is suspected; should always be obtained when the optic neuritis is bilateral and is obtained in most cases of optic neuritis in children
E. MRI of the spine with contrast if neurologic signs suggest spinal cord disease or if NMO is suspected
F. NMO antibodies: obtained in the serum of patients with bilateral optic neuritis, recurrent optic neuritis, severe optic neuritis with poor visual recovery, or when there is a spinal cord lesion or symptoms suggesting transverse myelitis
Explanation:
“8.4 Inflammatory Optic Neuropathy (Optic Neuritis)
Inflammation of the optic nerve is called optic neuritis. There are several different types of optic neuritis.
8.4.1 Characteristics
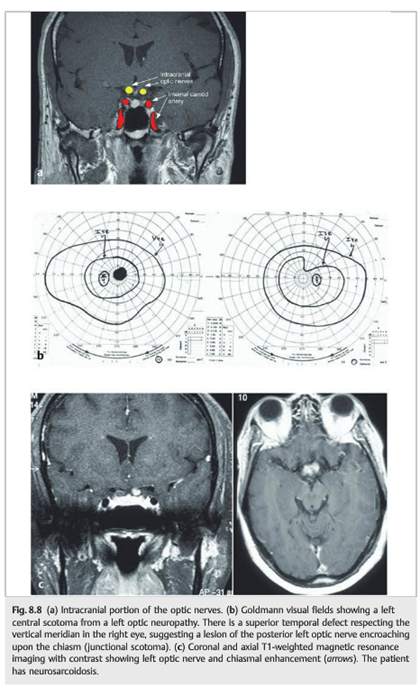
Optic neuritis is characterized by subacute, painful loss of central vision that may progress for 7 to 10 days (visual acuity varies from a mild reduction to severe loss); pain that is usually exacerbated by eye movement and may precede or coincide with visual loss; and abnormal color vision that is usually impaired out of proportion to visual acuity. Optic nerve appearance varies depending on which part of the optic nerve is inflamed. The term retrobulbar optic neuritis is used when the optic nerve appears normal in the acute phase. The terms anterior optic neuritis and papillitis are used when there is optic disc swelling. In both cases, temporal pallor of the disc develops 4to 6 weeks after visual loss. Optic nerve enhancement is often seen on orbital MRI.
8.4.2 Causes
There are multiple causes of optic neuritis, including infectious diseases, such as syphilis and cat scratch disease, and noninfectious inflammation, such as sarcoidosis. However, in most cases, optic neuritis remains idiopathic or is associated with multiple sclerosis. Optic neuritis may also be associated with other primary demyelinating diseases, such as NMO (Devic disease) and acute disseminated encephalomyelitis (ADEM).
8.4.3 Patient Evaluation
Evaluation of the patient includes checking for these characteristics:
● Cat exposure
● Recent travel
● Tick bite
● Immunosuppression
● Associated systemic symptoms and signs, including fever, lymphadenopathy, weight loss, skin lesions, cough, and arthralgias
● Associated neurologic symptoms and signs, including focal neurologic signs; a history of vertigo, diplopia, numbness, Lhermitte sign, or Uhthoff Phenomenon; headaches; and meningismus
● Associated ocular findings, including intraocular inflammation and retinitis.
The cause of optic neuritis is often suspected after the history and clinical examination.
Ancillary tests are obtained to confirm a presumed diagnosis.
Ancillary tests vary based on the foregoing evaluation and include the following:
● MRI of the brain and orbits with contrast (confirms optic nerve enhancement and looks for demyelinating disease in the brain)
● Chest radiograph (looking for sarcoidosis)
● Blood tests (vary based on presumed diagnosis): CBC, platelets, angiotensin-converting enzyme (ACE) level, and syphilis testing
● Lumbar puncture: performed when an infectious cause or underlying systemic inflammatory disease is suspected; should always be obtained when the optic neuritis is bilateral and is obtained in most cases of optic neuritis in children
● MRI of the spine with contrast if neurologic signs suggest spinal cord disease or if NO is suspected
● NMO antibodies: obtained in the serum of patients with bilateral optic neuritis, recurrent optic neuritis, severe optic neuritis with poor visual recovery, or when there is a spinal cord lesion or symptoms suggesting transverse myelitis
8.4.4 Classification
1. Optic neuritis associated with demyelinating disease
- Idiopathic optic neuritis
- Optic neuritis as a manifestation of any of the following:
○ Multiple sclerosis
○ NMO (Devic disease)
○ ADEM
2. Optic neuritis associated with infectious diseases
- Bacterial infections: syphilis, cat scratch disease (Bartonella henselae), Lyme disease, any bacterial meningitis, Mycoplasma pneumoniae, tuberculosis, Whipple disease (syphilis and cat scratch disease are the most common causes)
- Viral infections: herpes zoster, herpes simplex, HIV, Epstein–Barr virus, coxsackie virus, adenovirus, cytomegalovirus, hepatitis A and B virus, measles, mumps, rubella virus (herpes zoster is the most common cause)
- Parasitic infections: toxoplasmosis, cysticercosis, toxocariasis, intraocular nematode infection (toxoplasmosis is the most common cause)
- Fungal infections: cryptococcosis, aspergillosis, mucormycosis, histoplasmosis (cryptococcosis is the most common cause)
3. Post-vaccination optic neuritis
- Hepatitis B virus; rabies virus; tetanus toxoid; variola virus; combined smallpox, tetanus, and diphtheria vaccine; combined measles, mumps, and rubella vaccine; influenza vaccine; bacille Calmette-Guérin (BCG)
4. Optic neuritis associated with other inflammatory disorders
- Sarcoidosis
- Systemic lupus erythematosus
- Sjögren syndrome
- Polyarteritis nodosa
- Wegener granulomatosis
- Inflammatory bowel disease
- Behçet syndrome
- Bee and wasp stings
5. Isolated recurrent optic neuritis (autoimmune optic neuritis)”1
Reference:
1. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.