Questions:
1. What is the most common acute optic neuropathy in persons under the age of 45?
2. What is the most common cause of optic neuritis?
3. What condition is a common presenting sign of multiple sclerosis?
__________________________________________
Questions with answers:
1. What is the most common acute optic neuropathy in persons under the age of 45?
Idiopathic demyelinating optic neuritis is the most common acute optic neuropathy in persons under the age of 45.
2. What is the most common cause of optic neuritis?
Idiopathic demyelinating optic neuritis is the most common cause of optic neuritis.
3. What condition is a common presenting sign of multiple sclerosis?
Optic neuritis is a common presenting sign of multiple sclerosis.
Explanation:
“8.4.5 Idiopathic Demyelinating Optic Neuritis
Idiopathic demyelinating optic neuritis is the most common acute optic neuropathy in persons under the age of 45. It is also the most common cause of optic neuritis and often the presenting sign of multiple sclerosis.
Characteristics
Idiopathic demyelinating optic neuritis is more prevalent in young women than men (3:1). It is unilateral (occasionally bilateral) and is characterized by acute to subacute onset (usually rapidly progressive over a few days), decreased visual acuity (variable) and color vision (usually pronounced), pain with eye movements (in >90% of cases), and exacerbation with heat or exercise (Uhthoff Phenomenon).
Pearls
There is a strong association between optic neuritis and multiple sclerosis. Most patients with multiple sclerosis eventually have visual loss from optic neuritis. Many patients with acute isolated optic neuritis eventually develop multiple sclerosis.
Patient Evaluation
Examination should include the following:
● RAPD (if unilateral or asymmetric)
● Funduscopy:
○ Normal (two thirds of cases) or swollen (one third of cases) optic nerve head
○ Normal macula and retina (no exudates, no hemorrhages)
○ Optic disc pallor (only if at least 4–6 weeks after onset or if previous episode of optic neuritis)
● Visual field test:
○ Often central scotoma (diffuse depression on Humphrey visual field test)
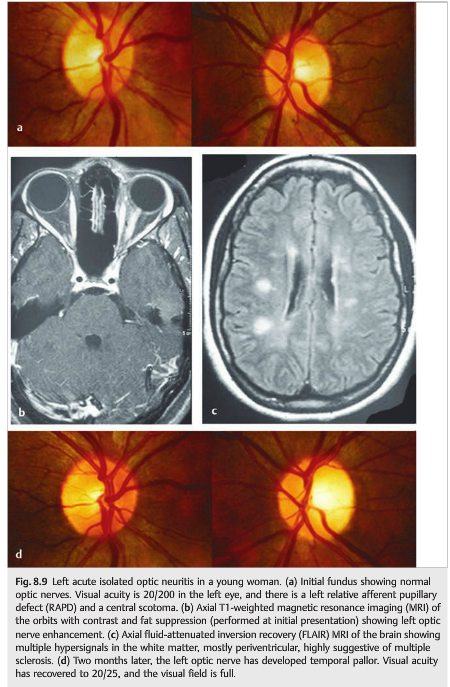
In >90% of cases, spontaneous improvement is seen within several weeks; the absence of improvement should raise concern for another diagnosis. Risk of multiple sclerosis (▶Fig. 8.9) should also be assessed.
Pearls
In >90% of patients with typical acute idiopathic demyelinating optic neuritis, visual acuity improves spontaneously to at least 20/40 at 6 months. The diagnosis should be reconsidered when the visual acuity does not improve.”1
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions, and corrections to tcooper@stanford.edu.