Questions:
1. Does the Transverse myelopathy of Neuromyelitis Optica (NMO) precede or follow the onset of optic neuritis?
2. Is there an antibody test for NMO?
3. What is the prognosis for NMO?
4. What are the diagnostic criteria for NMO?
 3
3
__________________________________________________________
Questions with answers:
1. Does the Transverse myelopathy of Neuromyelitis Optica (NMO) precede or follow the onset of optic neuritis?Either, the transverse myelopathy can precede or follows visual loss.
2. Is there an antibody test for NMO?
Yes, AQP4-IgG
3. What is the prognosis for NMO?
Poor
4. What are the diagnostic criteria for NMO?In 2015 new diagnostic criteria were introduced for neuromyelitis optica (NMO), and changed its name to neuromyelitis optica spectrum disorder (NMOSD).
NMOSD is an inflammatory disease of the central nervous system that can affect the optic nerves, brainstem, spinal cord, and brain. It can be mistaken for multiple sclerosis, but accurate diagnosis is essential because some drugs used for multiple sclerosis can worsen NMSOD.
The new core diagnostic clinical characteristics of NMSOG are:
- Optic neuritis
- Acute myelitis
- Area postrema syndrome: episode of otherwise unexplained hiccups or nausea and vomiting
- Acute brainstem syndrome
- Symptomatic narcolepsy or acute diencephalic clinical syndrome with NMOSD-typical diencephalic MRI lesions
- Symptomatic cerebral syndrome with NMOSD-typical brain lesions.
The new diagnostic criteria for NMOSD require at least one of the above core diagnostic clinical characteristic with a positive result on an antibody test (cell based assay recommended).
If the antibody test result is not positive, then the patient must have at least two core clinical characteristics (one of which must be optic neuritis, acute myelitis with longitudinally extensive transverse myelitis lesions, or area postrema syndrome) and must also show additional MRI requirements.
The additional MRI requirements are as follows:
- Acute optic neuritis: requires brain MRI showing (1) normal findings or only nonspecific white matter lesions or (2) optic nerve MRI with T2-hyperintense lesion or T1-weighted gadolinium enhancing lesion extending over 1/2 optic nerve length or involving optic chiasm
- Acute myelitis: requires associated intramedullary MRI lesion extending over three contiguous segments or at least three contiguous segments of focal spinal cord atrophy in patients with history compatible with acute myelitis
- Area postrema syndrome: requires associated dorsal medulla/area postrema lesions
- Acute brainstem syndrome: requires associated periependymal brainstem lesions
Explanation:
“NMO diagnostic criteria required optic nerve and spinal cord involvement but more restricted or more extensive CNS involvement may occur. The International Panel for NMO Diagnosis (IPND) was convened to develop revised diagnostic criteria using systematic literature reviews and electronic surveys to facilitate consensus. The new nomenclature defines the unifying term NMO spectrum disorders (NMOSD), which is stratified further by serologic testing (NMOSD with or without AQP4-IgG). The core clinical characteristics required for patients with NMOSD with AQP4-IgG include clinical syndromes or MRI findings related to optic nerve, spinal cord, area postrema, other brainstem, diencephalic, or cerebral presentations. More stringent clinical criteria, with additional neuroimaging findings, are required for diagnosis of NMOSD without AQP4-IgG or when serologic testing is unavailable. The IPND also proposed validation strategies and achieved consensus on pediatric NMOSD diagnosis and the concepts of monophasic NMOSD and opticospinal MS.”1
“NMO is associated with antibodies against the aquaporin-4 (AQP4) water channel.2 NMO–immunoglobulin G (IgG) predicts a relapsing course and is a supportive criterion for NMO.3–5 The high risk of relapse, sometimes with devastating effects, makes early diagnosis important. Early identification permits counseling and consideration for immunosuppressive therapy. The serum NMO-IgG assay, using indirect immunofluorescence, is 73% sensitive and 91% specific for clinically defined NMO.6 While helpful when positive, the sensitivity is insufficient to exclude the diagnosis. We describe 3 of 26 patients with NMO at our institution with NMO-IgG positivity restricted to CSF.”2
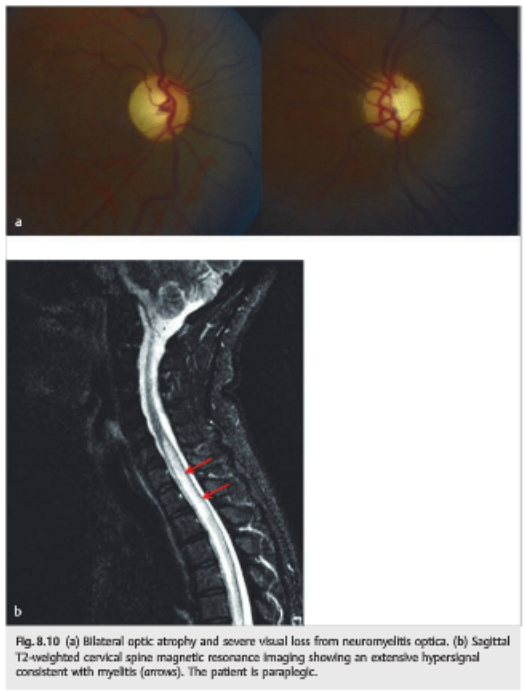
“8.4.6 Neuromyelitis Optica (Devic Disease)
The prognosis is usually poor, with permanent, severe visual loss and paraplegia.
…
Treatment usually consists of high-dose intravenous steroids followed by a slow taper of oral prednisone and long-term immunosuppressive therapy. Plasmapheresis is sometimes performed in cases with acute symptoms (▶Fig. 8.10).”3
References:
1. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Wingerchuk DM, et. al. Neurology. 2015:14; 85(2): 177–189.
2. NMO-IgG detected in CSF in seronegative neuromyelitis optica. Klawiter EC, et. al. Neurology. 2009; 72(12): 1101–1103.
3. Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.