Questions:
1. Are some maculopathies associated with mild optic nerve pallor?
2. Can maculopathies have dyschromatopsia?
3. In evaluating optic neuritis, when should a lumbar puncture for CSF analysis be considered?
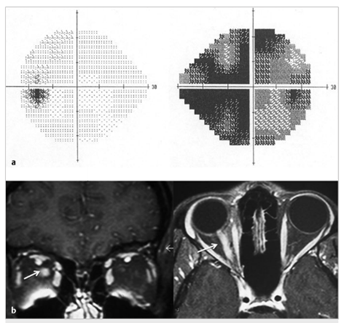
Fig.8.5
(a) Isolated right inflammatory optic neuropathy. There is a large central scotoma seen as diffuse depression on a 24–2 Humphrey visual field test.
(b)Coronal and axial T1-weighted magnetic resonance imaging with fat suppression and contrast showing enhancement of the orbital portion of the right optic nerve(arrow).
Questions with answers:
1. Are some maculopathies associated with mild optic nerve pallor?
Yes. Many chronic maculopathies are associated with mild optic nerve pallor.
2. Can maculopathies have dyschromatopsia?
Both Optic neuropathies and maculopathies cause central visual loss and dyschromatopsia.
3. In evaluating optic neuritis, when should a lumbar puncture for CSF analysis be considered?
Cerebrospinal fluid analysis may be helpful in cases of bilateral optic neuropathies, or when an infectious, systemic inflammatory, or neoplastic cause is suspected.
Explanation: Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
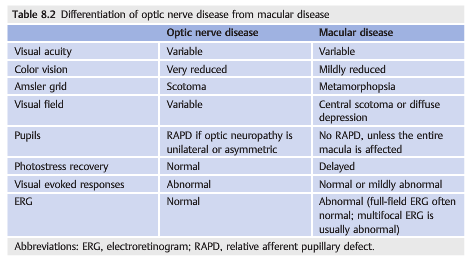
Optic neuropathies and maculopathies have overlapping presentations. Both cause central visual loss and dyschromatopsia. Many chronic maculopathies are associated with mild optic nerve pallor. When the macula appears normal, it may be difficult differentiate an optic neuropathy from a maculopathy (▶Table 8.2). Autofluorescence Imaging of the macula and spectral optical coherence tomography (OCT) are very helpful in distinguishing optic neuropathies from maculopathies when the macula appears normal on funduscopic examination.
8.3 Patient Evaluation
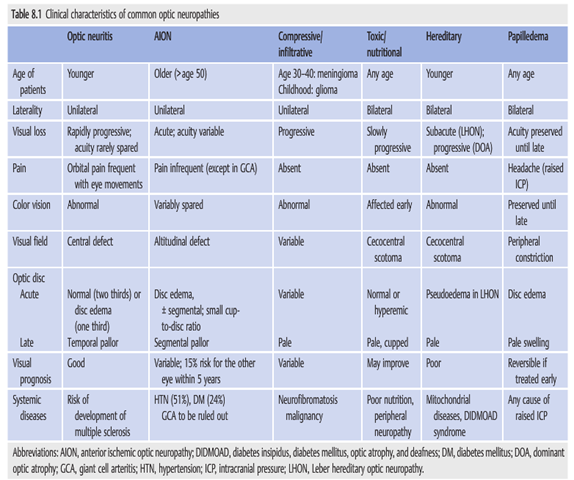
The following clinical characteristics are particularly helpful in determining the mechanism of the optic neuropathy:
● Mode of onset of visual loss
○ Acute (ischemic and inflammatory neuropathies)
○ Progressive (compressive or toxic optic neuropathies)
● Color vision (often relatively spared in ischemic optic neuropathies and usually very abnormal in inflammatory optic neuropathies)
● The presence of pain with eye movements (highly suggestive of an inflammatory in inflammatory optic neuropathies)
mechanism)
● Funduscopic appearance (variable in inflammatory optic neuropathies, reveals a swollen optic nerve in all cases of anterior ischemic optic neuropathy, and shows sometimes cupped optic nerve in compressive and hereditary optic neuropathies)
● Associated retinal changes in neuroretinitis
Evaluating the patient with suspected optic neuropathy includes the following:
1. Confirm the diagnosis of optic neuropathy by clinical examination.
2. Look for associated symptoms and signs.
3. Try to localize the optic nerve lesion (anterior, posterior in the orbit, orbital apex, or intracranial).
4. Determine the presumed etiologic diagnosis.
5. Obtain ancillary testing, such as imaging and laboratory workup, to confirm the diagnosis prior to initiating treatment.
Recommended tests include the following:
● Magnetic resonance imaging (MRI) of the brain and orbits with gadolinium (orbital images should be with fat suppression)
● Blood tests
○ Blood tests will vary, based on the presumed diagnosis.
○ Helpful tests include those for syphilis, sarcoidosis (angiotensin-converting enzyme[ACE]), cat scratch disease (Bartonella antibodies), Lyme disease, human immunodeficiency virus (HIV), inflammatory biologic syndrome (complete blood count[CBC], C-reactive protein [CRP], and erythrocyte sedimentation rate [ESR]),autoantibodies for autoimmune diseases (antinuclear antibodies [ANAs] and anti-neutrophil cytoplasmic antibodies [ANCAs]), and vitamin B12 and folate (bilateral and progressive painless optic neuropathies), as well as genetic testing for Leber Hereditary optic neuropathy (severe unilateral or bilateral optic neuropathies) and for dominant optic atrophy (bilateral and progressive painless optic neuropathies).
● Cerebrospinal fluid (CSF) (lumbar puncture)
○ Helpful in cases of bilateral optic neuropathies, or when an infectious, systemic inflammatory, or neoplastic cause is suspected.
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.