Question: What are 7 indications for B-scan echography?
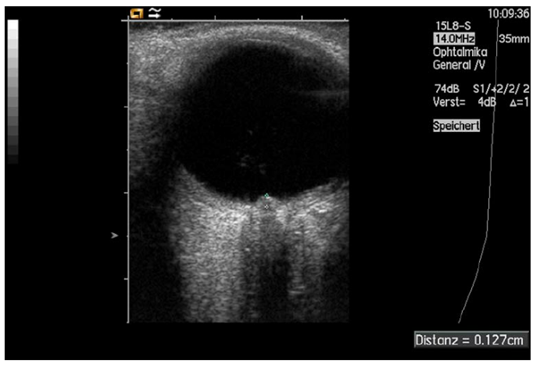
Fig. 8. Measurement of papilledema using ultrasound: disc elevation is quantified by putting the first caliper on the uppermost part of the swollen disc; the second caliper is positioned on the strongly reflecting line representing the lamina cribrosa 8
_____________________________________________
Question with answer: What are 7 indications for B-scan echography?
- Assessing the optic nerve head for buried drusen
- Trauma with poor view of the fundus to demonstrate vitreous hemorrhage or retinal detachment
- Identification of an intraocular foreign body
- Analysis of posterior pole tumors
- Examination of the extraocular muscles when thyroid eye disease is suspected
- Examination of the superior ophthalmic vein when a carotid-cavernous fistula is suspected
- Posterior scleritis (T-sign)
Explanation:
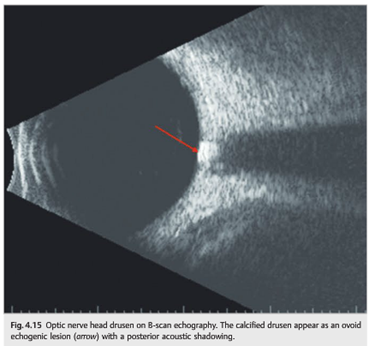
- Assessing the optic nerve head for buried drusen1
Optic nerve head drusen (may not be seen on fundus examination when buried)(▶Fig. 4.15)
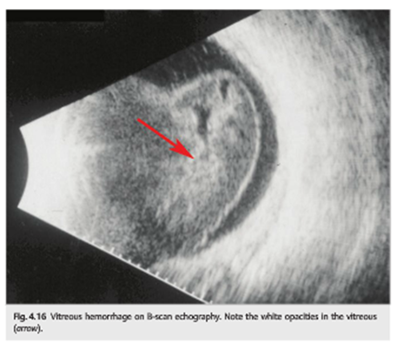
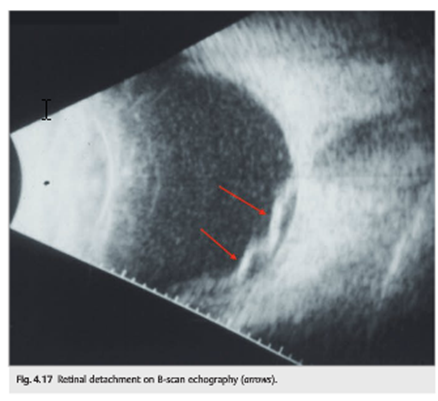
- Trauma with poor view of the fundus to demonstrate vitreous hemorrhage or retinal detachment1
Trauma with poor view of the fundus to demonstrate vitreous hemorrhage (▶Fig. 4.16)
or retinal detachment (▶Fig. 4.17)
- Identification of an intraocular foreign body
Computed tomography provides much more reliable information regarding the size, shape, and localization of the foreign body. MRI generally is not used in metallic IOFB. MRI may be more effective in localizing nonmetallic IOFB such as wood. Ultrasound can be a useful adjunct in localizing IOFB and to determine if the object is metallic. Ultrasound could be performed carefully in case of an open globe injury. Ultrasonography is useful in determining the extent of the intraocular damage, determining the presence of a retinal detachment, double perforation, as well as in detecting foreign bodies not seen on x-ray studies. Ultrasonography can give an idea about the nature of the IOFB such as round or spherical foreign bodies, intraocular air, glass etc. Ultrasound biomicroscopy is needed if FB in the angle is suspected.3
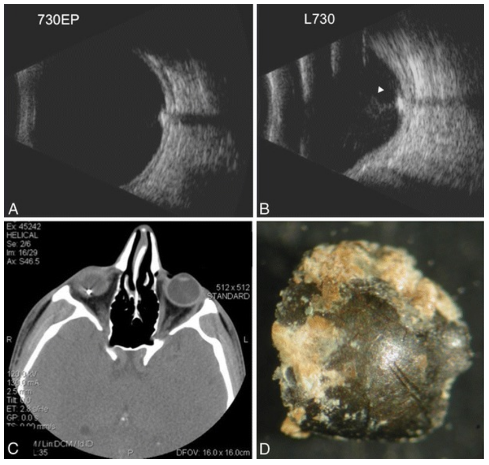
Figure 2: B-scan ultrasound of the right eye shows an intraocular foreign body (IOFB) with shadowing behind the IOFB on the 7:30 equator posterior (730EP) and 7:30 longitudinal (L730) scans (a, b). There is moderate vitreous debris overlying the IOFB but no distinct track in the vitreous (white arrow). (c) Axial CT scan confirms IOFB with metallic streaking artifact. (d) Gross photograph of metallic IOFB prior to inductively coupled mass spectrometry4 - Analysis of posterior pole tumors5
The most common tumor of the choroid is malignant melanoma. Although these can arise in the ciliary body or iris, they most commonly are seen in the choroid. Like retinoblastoma, ultrasound has become invaluable in the diagnosis and follow-up evaluation of uveal malignant melanomas. This homogenous highly cellular tumor results in low-to-medium internal reflectivity and regular internal structure. [3,9] Diagnostic A-scan and B-scan can detect internal vascularity in most melanomas.
A nearly pathognomonic finding is a collar button configuration (ie, mushroom shape), but this shape is seen in less than 25% of cases. Histologically, the collar button represents the portion of the tumor that has broken through the Bruch membrane, a basement membrane found between the choroid and the retina.
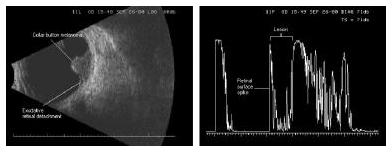
Collar-button shaped choroidal melanoma. The lesion began as a dome shape, then broke through the Bruch membrane to form the button on the anterior surface of the dome. Note the diagnostic A-scan pattern typical of melanoma, with the high retinal spike on the surface of the lesion but low-to-medium internal reflectivity within the lesion. The sclera and orbital tissues are seen as spikes to the right of the lesion. - Examination of the extraocular muscles when thyroid eye disease is suspected2
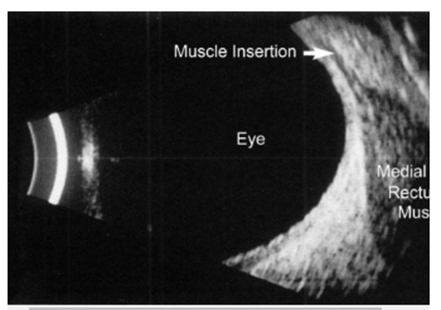
B-scan ultrasonogram reveals enlargement of the extraocular muscle belly. The tendinous insertion of the extraocular muscle at the globe is not thickened, which is characteristic of thyroid-related orbitopathy. - Examination of the superior ophthalmic vein when a carotid-cavernous fistula is suspected1
Examination of the superior ophthalmic vein when a carotid-cavernous fistula is suspected (▶Fig. 4.18)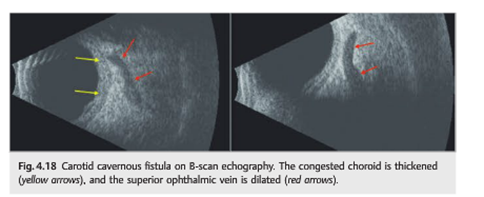
- Anterior and Posterior Scleritis
Scleritis usually presents with pain and redness that often awakens the patient FROM sleep. The conjunctival, episcleral, and scleral vessels are inflamed, leading to a bluish discoloration of the sclera. Scleritis is more common in women and is often unilateral. Work-up is routinely negative in the unilateral cases. B-scan ultrasonography shows diffuse thickening of the choroid, sclera, and episcleral tissues. Classically, the T-sign is present in cases of posterior scleritis. The T-sign is created by the fluid beneath Tenon’s capsule that creates a squaring off of the interface between the optic nerve and the sclera. Fluorescein angiography may SHOW punctate areas of leakage. The choroidal detachment is felt to be a result of the congested sclera. This congestion increases resistance to flow in the vortex veins and through the intact sclera, leading to choroidal effusions. 6
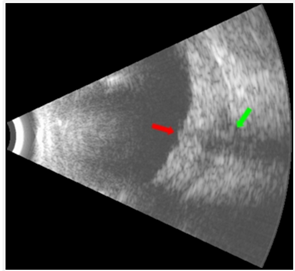
Fig. 6 B-mode ultrasonography showed diffuse thickening of the choroid, sclera and episcleral tissues. The thickness of the sclera-choroid complex measured 2.64 mm. The optic disc was swollen. There was fluid in the subtenon space producing a prominent T-sign (Figure 5). There was neither scleral nodule nor retinal detachment. The orbital veins were not dilated or tortuous. The T-sign was diagnostic of posterior scleritis.7
References:
- Neuro-ophthalmology Illustrated-2nd Edition. Biousse V and Newman NJ. 2012. Theme
- Imaging in Thyroid Ophthalmopathy. Medscape. 2016 http://emedicine.medscape.com/article/383412-overview
- Intraocular Foreign Bodies. Karth PA, Kamjoo S, Shah VA. EyeWiki. 2015
http://eyewiki.aao.org/Intraocular_Foreign_Bodies_(IOFB) - Occult intraocular foreign body masquerading as panuveitis: Inductively coupled mass spectrometry and electrophysiologic analysis. Yeh S, Ralle M, Phan I, Flaxel CJ. Journal of Ophthalmic Inflammation and Infection 2011 (2)35:99-103
- B-Scan Ocular Ultrasound. Waldron RG. Medscape 2016. http://emedicine.medscape.com/article/1228865-overview#showall
- Posterior Scleritis. Rudd JC. Digital Journal of Ophthalmology 1998 (4):20 http://www.djo.harvard.edu/print.php?url=/physicians/gr/317&print=1
- Posterior scleritis mimicking indirect carotid-cavernous fistula. Kah T, Premsenthil M, Salowi M, Thanaraj A, ak Gudom I. The Internet Journal of Ophthalmology and Visual Science. 2008 (7): 1 https://ispub.com/IJOVS/7/1/4930
- Application of Orbital Sonography in Neurology. Erlt M, Gamulescu MA, Schlachetzki F. Sonography 2012:203-216
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.