Question:
Which of the following are correct for a patient?
1. The eyes of a patient in coma will be closed.
2. Because the pathways governing ocular motility traverse the entire brainstem, brainstem lesions will most often result in abnormal eye movements, and the lesion can be localized to the midbrain, pons, or medulla.
3. The presence of a dysconjugate ocular deviation in coma (horizontal, vertical, or oblique misalignment) often indicates a cranial nerve palsy or skew deviation.
4. Roving eye movements: slow ocular conjugate deviations in random directions indicate intact ocular motility function in the brainstem.
5. Periodic alternating (“ping-pong”) gaze: slow, repetitive, rhythmic, back-and-forth, horizontal conjugate eye movements indicates intact ocular motility function in the brainstem.
6. Normal vertical and horizontal oculocephalic reflexes indicate intact ocular motility function in the brainstem.
 1
1
____________________________________________________
Correct Answers: all are correct
Explanation: “By definition, comatose patients have their eyes closed. They are unresponsive to all external stimuli, but there may be nonpurposeful movements or posturing of the limbs.
Coma results from the following:
● Direct brainstem-diencephalic damage disrupting the reticular formation or nuclei &
● Bilateral cerebral dysfunction
Some causes of coma include the following:
● Herniation from brain swelling or mass
● Hydrocephalus
● Intracranial hemorrhage
● Hypoxic-ischemic insult
● Trauma
● Infection
● Toxic/metabolic insult
When evaluating a patient with unexplained coma, differentiating between structural and toxic/metabolic causes is important, given that it influences workup and management.
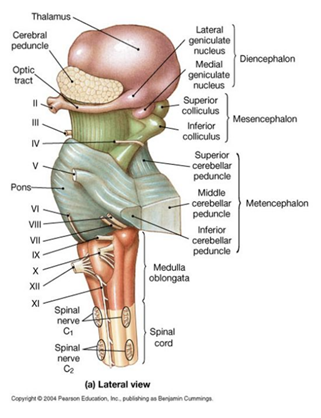
Neuro-ophthalmic examination is helpful, particularly regarding evaluation of the brainstem. Because the pathways governing ocular motility traverse the entire brainstem, brainstem lesions will most often result in abnormal eye movements, and the lesion can be localized to the midbrain, pons, or medulla; conversely, if the eye movements are normal, the brainstem is likely to be normal, and bilateral hemispheric or thalamic disease should be suspected.
Examination of the comatose patient involves the following:
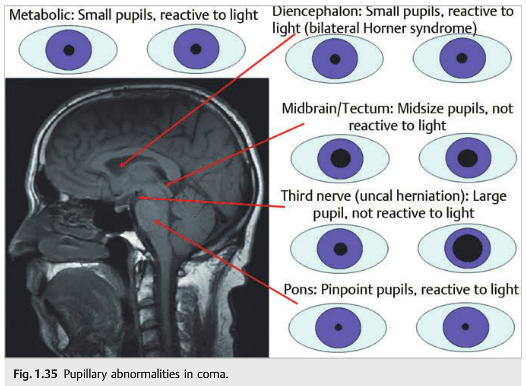
- Pupils (▶Fig. 1. 35): Metabolic causes of coma usually cause small reactive pupils. Many toxins and drugs administered may also have effects on the size of the pupils, and pharmacologic mydriasis can inadvertently occur in patients treated with aerosols after extubation.
○ Size
○ Shape
○ Reactivity to light - Eye position
○ Dysconjugate ocular deviation:
– Horizontal, vertical, or oblique misalignment
– Often indicates a cranial nerve palsy or skew deviation
○ Conjugate ocular deviation; conjugate lateral eye deviation indicates the following:
– Large lesion in the ipsilateral frontal lobe (the patient looks at his or her lesion)
– Lesion in contralateral pons (gaze palsy) (the patient looks away from the lesion)
– Seizure focus in the contralateral cerebral hemisphere
– Thalamic lesion, which may cause “wrong-way eyes,” with horizontal eye deviation paradoxically looking away from the lesion - Spontaneous eye movements
○ Roving eye movements: slow ocular conjugate deviations in random directions
– Indicate intact ocular motility function in the brainstem
○ Periodic alternating (“ping-pong”) gaze: slow, repetitive, rhythmic, back-and-forth, horizontal conjugate eye movements
– Indicates intact ocular motility function in the brainstem
○ Spontaneous nystagmus (unusual in coma)
○ Ocular bobbing: conjugate eye movement beginning with a fast downward movement followed by a slow drift back to the midline (similar to a fish bob in the water)
– Severe pontine lesion
○ Ocular dipping: slow downward movement followed by a quick upward deviation
– Severe pontine lesion
If there are no spontaneous eye movements, perform oculocephalic maneuvering (eliciting eye movements by turning the head horizontally, then vertically). The eyes should deviate in the direction opposite the head turn. This maneuver should NOT be performed in trauma patients with possible cervical spine injury.
In the comatose patient, cold caloric stimulation indicates a normal brainstem or bilateral hemispheric dysfunction when there is an ipsilateral tonic slow phase. It indicates a complete brainstem injury when there are no slow or fast eye movements.
Corneal reflex may be absent if there is pontine dysfunction.
Funduscopic examination of the comatose patient is usually performed undilated because pupil monitoring may be important in coma. Bilateral disc edema suggests raised intracranial pressure and should raise the possibility of an intracranial mass or hemorrhage, hydrocephalus, cerebral venous thrombosis, or meningitis.
Vitreous hemorrhage (uni- or bilateral) suggests Terson syndrome (related to acutely raised intracranial pressure, most commonly with subarachnoid hemorrhage). ”2
References:
1. The Brain (&CNS) Lecture 12a BIOL24 http://slideplayer.com/slide/6617555/ Anatomy: Brain Stem http://images.slideplayer.com/23/6617555/slides/slide_13.jpg
2. Neuro-ophthalmology Illustrated -2nd Edition. Biousse V and Newman NJ. 2012. Theme
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz. com.
Questions prior to September 2016 are archived at http://ophthalmology. stanford. edu/blog/
After that, questions are archived at https://neuro-ophthalmology. stanford. edu
Follow https://twitter. com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.