Questions:
1. A positive Hydroxyamphetamine pharmacologic test for Horner Syndrome indicates a problem in which neuron of the sympathetic chain?
a. 1st order neuron (preganglionic)
b. 2nd order neuron (preganglionic)
c. 3rd order neuron (postganglionic)
2. When the difference in dilation is + or < 0.5 mm. how reliable is the Hydroxyamphetamine pharmacologic test for Horner Syndrome?
a. sensitivity of 100% and specificity of 100%
b. sensitivity of 93% and specificity of 83%
c. sensitivity of 83% and specificity of 73%
d. sensitivity of 73% and specificity of 63
 1
1
__________________________________________
Answers:
1. c. 3rd neuron (postganglionic)
2. b. sensitivity of 93% and specificity of 83%
Explanation:
1. “Topical Hydroxyamphetamine is used to differentiate pre and postganglioninc Horner’s. Hydroxyamphetamine causes a release of norepinephrine from intact adrenergic nerve endings causing pupillary dilation. One hour after instillation of 1% hydroxyamphetamine eye drops dilation of both pupils indicate a lesion of the 1st or 2nd order neuron. If the smaller pupil fails to dilate it indicates a lesion of the 3rd order or postganglionic neuron
…
The etiology of Horner’s syndrome varies with the patient age and site of lesion. The etiology remains unknown in 35-40% of cases.
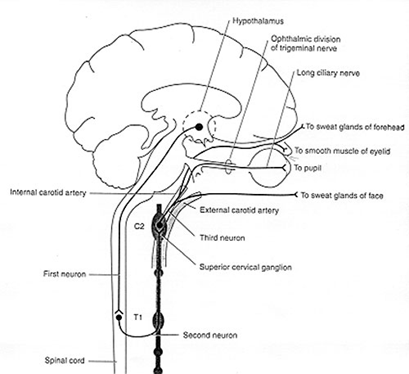
The pupil is innervated by sympathetic and parasympathetic fibers. Pupillary dilation is mediated by a three- neuron sympathetic pathway that originates in the hypothalamus.
The first order (central) neuron descends caudally from the hypothalamus to the first synapse in the cervical spinal cord (C8-T2 level-also called the ciliospinal center of Budge). The descending sympathetic tract is in close proximity to other tracts and nuclei in the brainstem.
The second order (preganglionic) neuron destined for the head and neck exits the spinal cord and travels in the cervical sympathetic chain through the brachial plexus, over the pulmonary apex and synapses in the superior cervical ganglion. The superior cervical ganglion is located near the angle of the mandible and the bifurcation of the common carotid artery.
The third order (postganglionic) neuron for the orbit enters the cranium within the adventitia of the internal carotid artery into the cavernous sinus. Here the oculosympathetic fibers exit the internal carotid artery in close proximity to the trigeminal ganglion and the sixth cranial nerve and join the 1st division of the trigeminal nerve to enter the orbit. The fibers (long ciliary nerve) innervate the dilator muscles of the iris and the Müller’s muscle in the upper and lower lid.
The vasomotor and sudomotor fibers to the face exit the superior cervical ganglion and ascend in the external carotid artery.
Pupillary constriction is produced by parasympathetic (cholinergic) fibers that travel with the third cranial (oculomotor) nerve.”2
 3
3
2. Hydroxyamphetamine mydriasis in Horner’s syndrome. 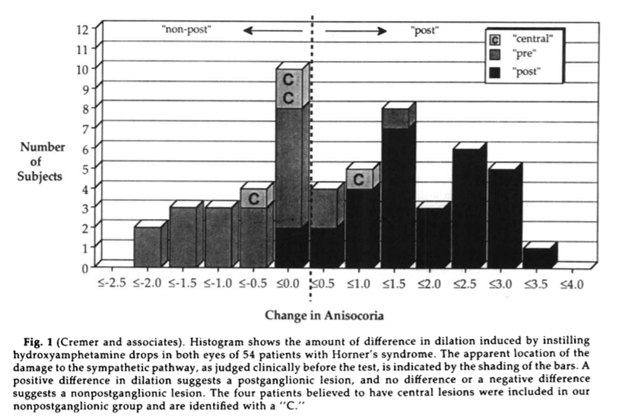
“The actual distributions of difference in dilation for our postganglionic and nonpostganglionic groups are shown in Figure 1. The division between the postganglionic and nonpostganglionic groups was not absolute; however, zero difference in dilation best distinguished the postganglionic and nonpostganglionic groups. With the dividing line in this location, a positive difference in dilation correctly identified the lesion as postganglionic in 88 % of the cases (positive predictive value = 88 %), and a known postganglionic lesion showed a positive difference in dilation 93% of the time (sensitivity = 93%). When the lesion was judged to be preganglionic or central (nonpostganglionic), the difference in dilation was negative or zero 83% of the time (specificity = 83%). When the difference was negative or zero, the lesion was nonpostganglionic 90% of the time (negative predictive value = 90%). A dividing line like this does not, however,convey all of the information.
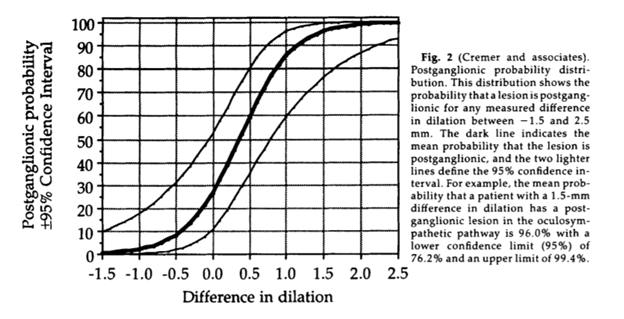
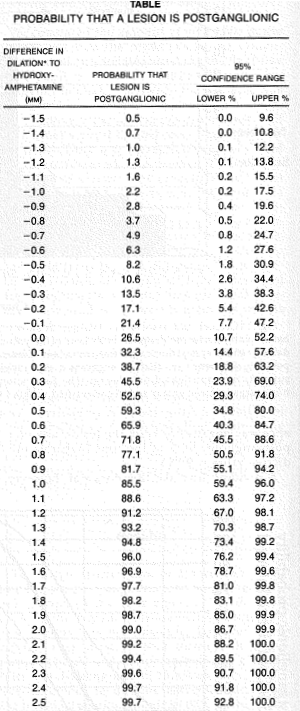
The clinician would like to know the likelihood that a patient with a given dilation difference has a postganglionic lesion. The results of the logistic regression analysis (Fig. 2 and the Table) provide this information and can help determine where the lesion is localized.
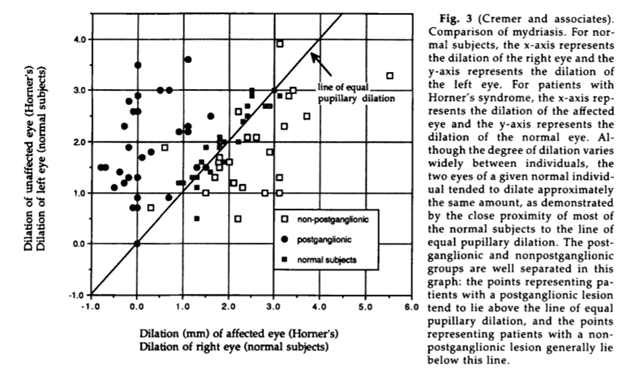
We also plotted the mydriasis of the affected eye against the mydriasis of the unaffected eye (Fig. 3). Included in Figure 3 are the data obtained from 26 normal subjects.’ In this graph, the division between postganglionic patients and nonpostganglionic patients can be seen, and the zone occupied by normal responses can be appreciated. A few patients with
Horner’s syndrome from both groups showed little asymmetry of mydriatic effect from hydroxyamphetamine, and their data overlapped the normative data. Additionally, two patients judged to have nonpostganglionic lesions showed an unexpected positive difference in dilation (Fig. 3). No patient thought to have a postganglionic lesion showed a negative difference in dilation (Fig. 3). Three patients, however,showed symmetric dilation, and one patient showed no hydroxyamphetamine effect in either eye.”4
“The pupillary response to hydroxyamphetamine eye-drops has been advocated as a test for subdividing patients with Horner’s syndrome into those with lesions of the 1st or 2nd sympathetic neuron (normal dilatation) and those with lesions of the 3rd neuron (no or minimal dilatation). We compared the response of the right and the left eye in 40 control subjects and also in 25 consecutive patients with Horner’s syndrome from a known lesion. In the controls, 1 eye might dilate up to 1.0 mm less than the other. In the patients, abnormally weak dilatation (difference with the other eye more than 1.0 ram) occurred only with lesions of the 3rd neuron, but in only 4 of 10 such cases. Of the other 6 patients with a lesion of the 3rd neuron 2 had a minimal response of the normal eye, and 4 showed subsequent recovery of oculosympathetic function (which suggests that denervation had not occurred). In conclusion, an abnormal hydroxyamphetamine test reliably indicates a lesion of the 3rd neuron, but a normal test provides little diagnostic aid.”5
References:
1. Horner’s syndrome. Physiopedia. http://www.physio-pedia.com/images/1/19/Horners.jpg
2. Horner’s syndrome. EyeWiki American Academy of Ophthalmology http://eyewiki.aao.org/Horner’s_syndrome#Pathophysiology
3. Understanding the anatomy of the sympathetic outflow tract is crucial. Neurologic Cases https://www.hopkinsarthritis.org/wp-content/uploads/2011/04/Slide-8-Brain-Schema.jpg
4. Hydroxyamphetamine mydriasis in Horner’s syndrome. Cremer SA, Thompson S, Digree KB, et al. Am J Ophthalmol 1990;110:71
5. Localization of Horner’s syndrome -Use and Limitations of the Hydroxyamphetamine Test. Van Der Wiel HL & Van Gun J. Journal of the Neurological Sciences, 1983, 59:229-235 229
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.