Questions:
1. How reliable is the Apraclonidine pharmacologic test for
Horner Syndrome?
a. less reliable than cocaine
b. at least as reliable as cocaine
c. more reliable than cocaine
2. In children up to what age may Apraclonidine cause lethargy, bradycardia, or a reduced respiratory rate for up to 2 hours?
a. 3 months
b. 6 months
c. 1 year
d. 2 years
1
__________________________________________
Correct Answers:
Question 1. b. at least as reliable as cocaine
Question 2. b. 6 months
Explanation:
1. The sensitivity and specificity of 0.5% apraclonidine in the diagnosis of oculosympathetic paresis.
Aims: To evaluate the sensitivity and specificity of 0.5% apraclonidine test in the diagnosis of oculosympathetic paresis (OSP).
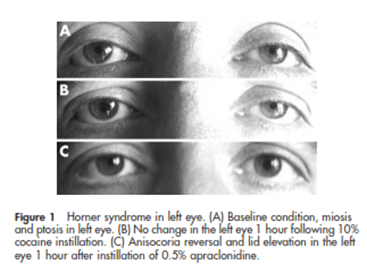
Method: Apraclonidine (0.5%) was administered to 31 eyes, nine with a diagnosis of Horner syndrome (HS), 22 with bilateral OSP caused by diabetes, and to 54 control eyes. All were confirmed with the cocaine test. The effects on pupil diameter and upper eyelid level were observed 1 hour later.
Results: Apraclonidine caused a mean dilation of 2.04 mm (range 1–4.5) (p<0.001) in the pupils with OSP and it caused pupillary constriction in the control eyes with a mean change of -0.14 mm (range 0.5-1) (p<0.05). It caused reversal of anisocoria in all HS cases. Its effects on both pupil diameters and upper lid levels differed significantly between the groups (p<0.001). The mean elevation in the upper lid was 1.75 mm (range 1–4) in the OSP group (p<0.001) and 0.61 mm (range 0–3) in the control group (p<0.001).
Conclusion: The effect of the apraclonidine (0.5%) test on the pupil diameter was diagnostic for OSP and had at least the same sensitivity and specificity as the cocaine test for the diagnosis of OSP.
2. Adverse effects of apraclonidine used in the diagnosis of Horner syndrome in infants.
The reported adverse effects included in this report suggest that apraclonidine should be used with caution or not at all, in infants under the age of 6 months. Though a reduced concentration of apraclonidine (0.5%) is also effective in the diagnosis of Horner syndrome,it is the immaturity of the blood-brain barrier in young infants that permits central nervous system depression suggesting that patients may still be at risk. If apraclonidine must be used in infants younger than 6 months of age, the patient should be observed for a period of at least 2 hours after instillation of the drops, with admission to a pediatric ward prompted by lethargy, bradycardia, or a reduced respiratory rate.
References:
1. The sensitivity and specificity of 0.5% apraclonidine in the diagnosis of oculosympathetic paresis. F Koc, S Kavuncu, T Kansu, G Acaroglu, E Firat. Br J Ophthalmol 2005;89:1442–1444.
2. Adverse effects of apraclonidine used in the diagnosis of Horner syndrome in infants. Watts S, et al. Journal of AAPOS 2007:11(3):282-283
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.