Question:
1.What is the effect of the following agents on the pupils in Horner Syndrome?
Cocaine
Hydroxyamphetamine
Apraclonidine
2. What is the mechanism of action of each of these agent used to test Horner Syndrome?
Cocaine
Hydroxyamphetamine
Apraclonidine
 1
1
__________________________________________
Correct Answers:
Question 1.
Cocaine – the affected eye fails to dilate as well as the normal eye dilates, resulting in at least 1 mm of anisocoria within 45 minutes after instillation.
Hydroxyamphetamine – causes dilation of the pupil as long as the third-order neuron is intact. Prompt dilation occurs in a normal eye but also in an eye with a preganglionic Horner’s syndrome. Failure to dilate suggests that the presynaptic bulb has degenerated secondary to a lesion of the third-order neuron. A false-negative test can occur if the test is performed too soon after a third-order neuron insult, before atrophy of the presynaptic bulb has occurred. The test is generally considered accurate after the symptoms have been present for 2 to 3 weeks.
Apraclonidine – dilates the Horner’s pupil but has no significant effect on the normal pupil. It reverses the anisocoria.
Question 2.
Cocaine – Blocks the normal reuptake of norepinephrine, allowing norepinephrine to accumulate in the synaptic cleft which dilates the pupil if norepinephrine is present.
Hydroxyamphetamine – causes the release of norepinephrine into the synaptic cleft at the neuromuscular junction, independent of any neural signal. No norepinephrine will be present in the case or a lesion of the 3rd order neuron. Prompt dilation occurs in a normal eye but also in an eye with a preganglionic Horner’s syndrome. Failure to dilate suggests that the presynaptic bulb has degenerated secondary to a lesion of the third-order neuron. A false-negative test can occur if the test is performed too soon after a third-order neuron insult, before atrophy of the presynaptic bulb has occurred. The test is generally considered accurate after the symptoms have been present for 2 to 3 weeks.
Apraclonidine – Upregulation of post-junctional alpha-1 receptors in denervated sympathetic pupillary dilator muscles produced a pharmacologic supersensitivity in affected eyes to apraclonidine.
Explanation:
 2
2
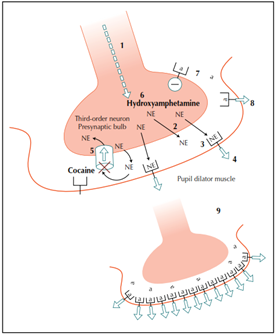
Figure 1.
“Cocaine – Norepinephrine is the neurotransmitter at the neuromuscular junction of the sympathetic third-order neuron and the iris dilator muscle (Fig. 1). In the normal state there is a continuous release of norepinephrine from the presynaptic terminal due to baseline sympathetic tone. The neurotransmitter is continuously degraded by reuptake at the presynaptic nerve terminal. Topical cocaine blocks the reuptake of norepinephrine, causing an accumulation of the neurotransmitter in the synaptic cleft, which produces dilation of a normal pupil. If sympathetic tone is lacking and there is little or no baseline release of norepinephrine into the cleft, then cocaine is an ineffective dilator. Thus topical cocaine can be used to detect a deficiency of sympathetic tone caused by a defect at any point in the sympathetic chain. The test is therefore “positive” for Horner’s syndrome if the affected eye fails to dilate as well as the normal eye dilates, resulting in at least 1 mm of anisocoria within 45 minutes after instillation [52]. If both pupils dilate equally well then an oculosympathetic paresis is unlikely. However, cocaine will also fail to dilate pupils that are otherwise incapable of dilating, such as an atrophic iris, or an iris with posterior synechiae or iris neovascularization. Thus, there are potential false-positive situations inherent in this test, especially if a slit-lamp examination of the iris is not performed. A mild reversal of the ptosis may be noted with cocaine drops, but this finding is usually subtle and not clinically useful.
Hydroxyamphetamine – Hydroxyamphetamine hydrobromide 1% (previously available as Paredrine; Smith Kline & French, Philadelphia, PA) acts by forcing the release of norepinephrine into the synaptic cleft at the neuromuscular junction, independent of any neural signal (Fig. 1). This causes dilation of the pupil as long as the third-order neuron is intact. Prompt dilation occurs in a normal eye but also in an eye with a preganglionic Horner’s syndrome. Failure to dilate suggests that the presynaptic bulb has degenerated secondary to a lesion of the third-order neuron. A false-negative test can occur if the test is performed too soon after a third-order neuron insult, before atrophy of the presynaptic bulb has occurred. The test is generally considered accurate after the symptoms have been present for 2 to 3 weeks [53]. Like cocaine testing, a drop is placed in both eyes, with the unaffected eye serving as a control (Table 1).
In congenital Horner’s syndrome, preganglionic lesions may produce orthograde transsynaptic failure of the postganglionic oculosympathetic neuron. The hydroxyamphetamine test may therefore fail to dilate such a pupil, falsely localizing a lesion as postganglionic. The hydroxyamphetamine test may therefore be misleading in infants with Horner’s discovered during the first year of life [54,55].
Apraclonidine – Apraclonidine (Iopidine; Alcon, Fort Worth, TX) is a direct alpha-adrenergic receptor agonist that lowers intraocular pressure by reducing aqueous production. In normal eyes, apraclonidine has no appreciable effect on pupil size. However, Morales et al. [57] reported that 1% apraclonidine dilated the pupil in eyes with unilateral Horner’s syndrome. Patients with Horner’s syndrome were chosen for this glaucoma study because apraclonidine’s effect on intraocular pressure could be assessed without the potentially confounding systemic effect of oculosympathetic tone. The study showed that apraclonidine successfully lowered the pressure in both affected and normal eyes, and they concluded that the drug’s effect was indeed at the post-junctional alpha-2 receptors of the ciliary body, and any systemic effect (via oculosympathetic efferents) on intraocular pressure was negligible. Pupillary size was initially of secondary interest. However, the study showed that apraclonidine reliably dilated the Horner’s pupil but had no significant effect on the normal pupil. In fact, apraclonidine reversed the anisocoria in all six patients with Horner’s syndrome in this study (four were postganglionic, two were preganglionic). They proposed that the upregulation of post-junctional alpha-1 receptors in denervated sympathetic pupillary dilator muscles produced a pharmacologic supersensitivity in affected eyes. In normal eyes, any small degree of alpha-1 activity that might tend to dilate the pupil would be offset by apraclonidine’s presynaptic alpha-2 activity, which tends to downregulate the production and release of norepinephrine. In eyes with Horner’s syndrome, the activity becomes clinically visible with upregulation from denervation hypersensitivity, and loss of sympathetic tone negates the effect of further inhibition from alpha-2 activity. This study was the first to suggest that apraclonidine may indeed have clinical diagnostic value for Horner’s syndrome [57].
…
Apraclonidine did reverse the ptosis in the majority of patients with Horner’s syndrome, but it also elevated the eyelids in 45% of normal eyes. Thus, reversal of ptosis with apraclonidine is not useful in diagnosis but may be a consideration for symptomatic relief in patients with Horner’s syndrome [63,66].”2
Reference:
1. Horner’s syndrome, Pseudo-Horner’s syndrome, and simple anisocoria. Martin TJ. Curr Neurol Neurosci Rep. 2007 Sep;7(5):397-406
2. Horner syndrome cat image. http://kingstonah.com/blog/wp-content/uploads/2015/11/2552587598_dc0cbde2e8_b.jpg
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.