 4
4
Question: Which of the following may cause anisocoria?
1. Normal physiology
2. A deficit of sympathetic innervation
3. A deficit of parasympathetic innervation
4. 3rd nerve paresis
5. Trauma
6. Congenital anomalies
7. Pharmacologic agents
8. Exposure to plant material
____________________________________________
Correct Answers: Anisocoria may be do to any of these items.
Explanation3: “Generally, anisocoria is caused by impaired dilation (a sympathetic response) or impaired constriction (a parasympathetic response) of pupils. An injury or lesion in either pathway may result in changes in pupil size.
Physiologic (also known as simple or essential) anisocoria is the most common cause of unequal pupil sizes, affecting up to 20% of the population.[1] It is a benign condition with a difference in pupil size of less than or equal to 1 mm.[2] The exact cause is unknown, but it is thought to be due to transient asymmetric supranuclear inhibition of the Edinger-Westphal nucleus that controls the pupillary sphincter.[3] Light and near responses is intact, and the degree of anisocoria is typically equal in light and dark. Physiologic anisocoria may be intermittent and even self-resolving. However, many cases are persistent.
Congenital anomalies in the structure of the iris may contribute to abnormal pupillary sizes and shapes that present in childhood. Examples include aniridia, coloboma and ectopic pupil.
Mechanical anisocoria is an acquired defect that results from damage to the iris or its supporting structures. Causes include physical injury from ocular trauma or surgery, inflammatory conditions such as iritis or uveitis, angle closure glaucoma leading to iris occlusion of the trabecular meshwork, or intraocular tumors causing physical distortion of the iris.
Pharmacologic anisocoria can present as mydriasis or miosis following administration of agents that act on the pupillary dilator or sphincter muscles. Anticholinergics such as atropine, homatropine, tropicamide, scopolamine and cyclopentolate lead to mydriasis and cycloplegia by inhibiting parasympathetic M3 receptors of the pupillary sphincter and ciliary muscles. The use of pilocarpine, a non-selective muscarinic receptor agonist in the parasympathetic nervous system, may result in a small and poorly reactive pupil. Sympathomimetics such as adrenaline, and phenylephrine cause mydriasis through their actions at ɑ-1 receptors of the pupillary dilator muscle.
Horner’s syndrome (oculosympathetic palsy) is classically described by the triad of ptosis, miosis and anhydrosis, although clinical presentation may vary. Anisocoria is greater in the dark due to a defect in the pupillary dilator response secondary to lesions along the sympathetic trunk. Central or first-order lesions are often caused by stroke, lateral medullary syndrome, neck trauma or demyelinating disease. Preganglionic or second-order neuron lesions may be caused by a Pancoast tumor, mediastinal or thyroid mass, cervical rib, and neck trauma or surgery. Postganglionic or third-order neuron lesions include carotid artery dissection, cavernous sinus lesion, otitis media, and head or neck trauma. Further pharmacologic workup (see diagnostic procedures) is useful in confirming Horner’s and distinguishing the order of the lesion.
Adie’s tonic pupil results from damage to the parasympathetic ciliary ganglion or short ciliary nerves that innervate the sphincter pupillae and ciliary muscle. Aberrant reinnervation and upregulation of post-synaptic receptors lead to the clinical presentation of a tonically dilated pupil with near stimulation that is poorly reactivity to light. Ninety percent of cases occur in women between the ages of 20-40 years, 80% of cases are unilateral, and 70% of cases are associated with decreased deep tendon reflexes (Adie’s syndrome).[2]
Oculomotor (third) nerve palsy varies in presentation and etiology. The oculomotor nerve innervates 4 out of the 6 extraocular muscles (superior rectus, medial rectus, inferior rectus and inferior oblique), the sphincter pupillae muscle, the ciliary muscle and the levator palpebrae muscle. Third nerve palsies rarely present as an isolated mydriasis; associated findings include ptosis, an ipsilateral “down and out” gaze, and loss of accommodation. Compressive lesions from head trauma, intracranial aneurysms, uncal herniation and tumors typically involve the pupil as they affect the superficial parasympathetic fibers that innervate the pupil. Ischemic or diabetic oculomotor nerve palsies typically spare the pupil.[4]”
“A careful history to elucidate the onset and chronicity of anisocoria may be useful for determining its etiology. Old photographs may provide information since symptoms may not exist or may go unnoticed. Chronic anisocoria without associated symptoms may point to a benign process such as physiologic anisocoria, whereas sudden-onset anisocoria in the setting of other symptoms may be more worrisome. For example, anisocoria with headaches, confusion, altered mental status and other focal neurologic deficits suggest an underlying mass effect and may require further neurologic work-up and intervention.
Complete ophthalmic history is important as coexisting ocular conditions, previous surgeries or trauma to the head or orbit may also contribute to anisocoria. A thorough review of medications, especially topical eye drops, may provide explanations for pharmacologic anisocoria. A discussion about exposures to certain narcotics, insecticides (organophosphates) or plants (Brugmansia Angel’s trumpet or Datura Devil’s trumpet), should also be considered.”
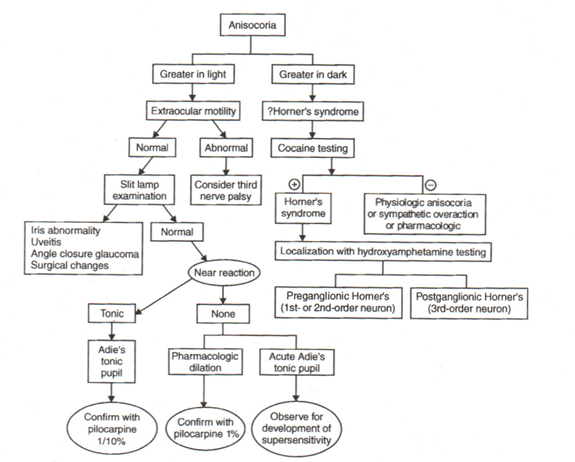
Anisocoria Care Path2
From: Clinical Pathways in Neuro-ophthalmology 2003
References:
1. Clinical Decisions in Neuro-Ophthalmology, Burde RM, Savino PJ & Trobe JD. 3nd Edition. Mosby 2002
2. Clinical Pathways in Neuro-ophthalmology:An Evidence-Based Approach. Lee AC & Brazis PW. Thieme 2003
3. EyeWiki Anisocoria. Boisvert JC. 2016 http://eyewiki.aao.org/Anisocoria
4. The Eyes Have It – Anisocoria http://kellogg.umich.edu/theeyeshaveit/symptoms/images/anisocoria.jpg
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.