Question: Describe the appropriate steps to take in evaluating visual field loss in the emergency department.
 4
4
__________________________________________
ED Concerns: stroke, intracranial infiltrative and mass lesions, pituitary apoplexy
ED Evaluation:
1. Perform confrontation VFs – test each eye with finger counting in each quadrant of the visual field and test the far periphery with finger motion.
2. If the visual field affects only one eye
A. Evaluate for intraocular cause
a. Amsler grid and photo stress test to rule-out subtle macular disease
b. Swinging flashlight test to screen for optic neuropathy – RAPD present assess for optic neuropathy
c. Intraocular examination
– Findings of central or branch artery occlusion
– – Central artery occlusion – Provide immediate treatment to lower IOP
– – Central or branch retinal artery occlusion initiate ED Stroke evaluation protocol.
– Findings of optic disc edema with a macular star present
– Obtain blood tests for Bartonella henselae and Lyme disease
– Consider acute idiopathic blind spot syndrome (AIBSE)3
3. If the visual field affects both eyes
A. If the defect is of possible recent onset, initiate ED Stroke evaluation protocol.
B. Obtain emergent brain MRI with and without contrast including diffusion weighted images.
C. Consider pituitary apoplexy in your differential diagnosis:
Classical pituitary apoplexy: clinical features, management and outcome. Randeva HS, etal. Clin Endocrinol (Oxf). 1999 Aug;51(2):181-8.
“Patients were followed for up to 11 years (mean 6.3 years: range 0.5-11).
Headache (97%) was the commonest presenting symptom, followed by nausea (80%) and a reduction of visual fields (71%).
MRI correctly identified pituitary haemorrhage in 88% (n = 7), but CT scanning identified haemorrhage in only 21% (n = 6)”
D. Arrange neuro-ophthalmology clinic follow-up with scheduled formal visual fields – symptoms within 30° schedule for HVF 30-2, outside 30°schedule for GVF.
Explanation:
Co-occurrence of Acute Retinal Artery Occlusion and Acute Ischemic Stroke-Diffusion-weighted MRI study. Lee J, et al. AJO. 2014:157(6):1231-1238
PURPOSE: To evaluate the co-occurrence of acute ischemic stroke and acute retinal artery occlusion (RAO).
DESIGN: Retrospective observational case series.
METHODS: We included 33 consecutive patients with acute RAO who underwent diffusion-weighted magnetic resonance imaging within 7 days of the onset of visual symptoms. The causes of RAO were classified according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria, which are based on clinical features and the results of etiological evaluations for atherosclerosis, cardioembolism and other prothrombotic conditions. We evaluated the prevalence of accompanying acute ischemic stroke in subjects with acute RAO and examined the relationships with etiological parameters.
RESULTS: Acute ischemic stroke was detected in 8 (24.2%) subjects with RAO. Among these subjects, 3 (37.5%) patients did not exhibit any neurologic symptoms or signs. Most of the infarction patterns were small, multiple and scattered. All of the subjects with RAO who were positive for lesions on diffusion-weighted imaging had identifiable causes, whereas only 36% of the subjects who were negative for lesions had identifiable etiologies (P = .003). Carotid stenosis or cardioembolic sources were found more commonly in cases of central retinal artery occlusion (CRAO; 7/18, 38.9%) than in cases of branch retinal artery occlusion (BRAO; 1/15 6.7%, P = .046).
CONCLUSIONS: Acute cerebral infarctions frequently accompany RAO. We recommend diffusion-weighted imaging for patients with RAO because the presence of lesions on diffusion-weighted imaging is accompanied by a significantly increased probability of identifying the cause.
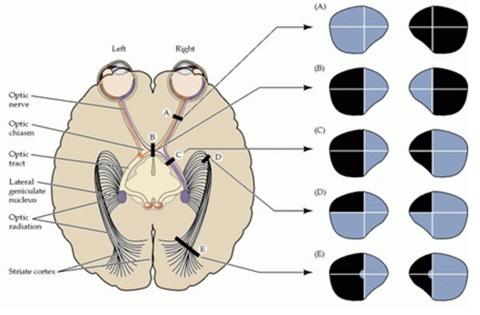
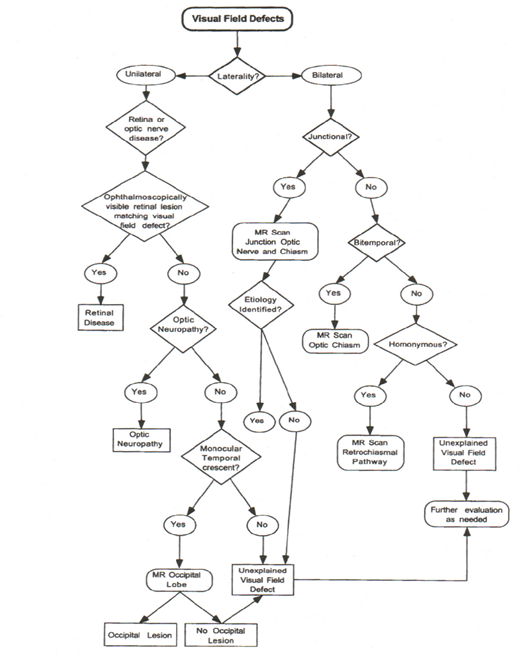
Visual Field Defect Care Path
From: Clinical Pathways in Neuro-ophthalmology 2003
References:
1. Co-occurrence of Acute Retinal Artery Occlusion and Acute Ischemic Stroke-Diffusion-weighted MRI study. Lee J, et al. AJO. 2014:157(6):1231-1238
2. Clinical Decisions in Neuro-Ophthalmology, Burde RM, Savino PJ & Trobe JD. 3nd Edition. Mosby 2002
3. Clinical Pathways in Neuro-ophthalmology:An Evidence-Based Approach. Lee AC & Brazis PW. Thieme 2003
4. Visual Field Defect Lesion Locations http://www.psychologyus.com/images/Visualdeficit1_450x316.jpg
More than 600 additional neuro-ophthalmology questions are freely available at http://EyeQuiz.com.
Questions prior to September 2016 are archived at http://ophthalmology.stanford.edu/blog/
After that, questions are archived at https://neuro-ophthalmology.stanford.edu
Follow https://twitter.com/NeuroOphthQandA to be notified of new neuro-ophthalmology questions of the week.
Please send feedback, questions and corrections to tcooper@stanford.edu.